|
© Borgis - Postępy Nauk Medycznych 10, s. 739-743
*Eberhard Ritz
Prenatal Programming – impact on the kidney and beyond**
Rozwój narządów w życiu płodowym – wpływ na stan nerek
Ruperto-Carlola-University Heidelberg (Germany)
Streszczenie
There is increasing evidence that prenatal programming accounts, at least in part, for a large segment of hypertension, particularly salt sensitive hypertension and albuminuria as well as chronic kidney disease. Apart from this it also predisposes to the metabolic syndrome which may explain the high cardiovascular risk in patients with chronic kidney disease. Słowa kluczowe: prenatal programming, epigenetic factors, birth weight, salt sensitive hypertension, chronic kidney disease, metabolic syndrome
Summary
W ostatnich latach wykazano, że nieprawidłowy rozwój narządów w życiu płodowym może uczestniczyć w istotny sposób w patogenezie nadciśnienia tętniczego, zwłaszcza sodozależnego, albuminurii oraz przewlekłej choroby nerek u osób dorosłych. Ponadto nieprawidłowe programowanie rozwoju narządów w życiu płodowym może również predysponować do rozwoju zespołu metabolicznego, który to z kolei może tłumaczyć zwiększone ryzyko powikłań sercowo-naczyniowych u chorych z przewlekłą chorobą nerek. Key words: programowanie płodowe, czynniki epigenetyczne, nadciśnienie sodozalezne, przewlekła choroba nerek, zespół metaboliczny
Laudatio dedicated to Professor emeritus Prof. Francicek Kokot
Professor Franciszek Kokot was born on November 24th, 1929 in Olesno Slaskie and will soon celebrate his 80th birthday. On this occasion, German nephrologic colleagues send their best wishes. We are full of admiration to see the gigantic achievements of the pioneer in clinical nephrology who covered the breadth of our specialty, a true ”uomo universale”.
This achievement is all the more admirable, since it was achieved under the most difficult conditions before the implosion of the Eastern Block.
What we in Germany particularly appreciated was his effort early on to maintain contacts with neighbouring countries including Germany. The German Society (Gesellschaft für Nephrologie) recognized this by the honorary membership for Franciszek Kokot in 1979. He was able to overcome the barriers existing in the past between Eastern and Western countries. This is reflected, amongst others, by his very successful scientific collaboration with several German groups involved in renal research. He initiated a very fruitful exchange of collaborators and several of his fellows spend some time in our country. It is common scientific work and mutual collaboration across frontiers which help to overcome bitter pages in our history.
Franciszek Kokot has achieved international recognition and served as an officer in a number of international societies, particularly the European Renal Association (EDTA-ERA) and the International Society of Nephrology (ISN).
He was highly respected as an expert in renal research and this is reflected, amongst others, by his membership in numerous editorial boards, including Kidney International, Nephrology Dialysis Transplantation, Clinical Nephrology and Nieren- und Hochdruckkrankheiten.
In old German academic tradition we wish the still sprightly octogenarian ” ad multos annos ”.
Introduction
In the recent past is has increasingly been appreciated that prenatal causes account to considerably extent for chronic kidney disease. This concept goes back to past epidemiological observations which showed a relation between adult pathology and birth weight as well as conditions in early childhood. This prompted B. Brenner to propose the following hypothesis: restricted growth in utero and low birth weight cause hypertension as well as increased renal risk at adult age the common link being a lower endowment of nephrons at the time of birth.
The molecular mechanisms explaining the counterintuitive fact that the same genome will result in differing phenotypes depending on intrauterine conditions have recently been lucidly explained by the concept of ”epigenetics”, i.e. that the read-off from the primary DNA code is modulated by covalent changes in histones and DNA respectively: transcription of the genetic code is modulated by covalent modification of histones (methylation or acetylation and desmethylation or desacetylation respectively), favouring or impeding access to coding DNA. In addition methyltransferases, methylating CpG sequences, play a role amongst others in silencing genes.
Numerous animal experiments have shown that maternal pathology may impair nephrogenesis of the offspring, e.g. low protein intake, uterine underperfusion, maternal hyperglycemia, maternal hyperinsulinemia, high and low maternal salt intake as well as exposure to corticosteroids to name only a few.
Adverse intrauterine milieu causes ”nephron underdosing”
The classical studies of Oliver (The Kidney and Nephrons; Harper and Row; 1968) showed a wide variation of nephron numbers in humans at autopsy, ranging from 800 000 to 1.8 million per kidney. Manalich examined the kidneys of low birth weight newborns: the number of glomeruli was less, but their volume was larger. Recently available technologies of in vivo evaluation of kidney growth documented that children born with low birth weight have low kidney volume. This can today be monitored by sonography even in utero where small and ”sausage shaped” foetal kidneys point to impaired cell and tissue migration.
Low birth weight is associated with high blood pressure later in life even when adjustments are made for current weight. The final outcome is the end result of two processes: low birth weight on the one hand (which accounts for higher adolescent blood pressure by 2-3 mm Hg) and higher catch up growth leading to adult fatness and overweight on the other hand (further aggravating hypertension). This relation between birth weight and blood pressure has also been documented in individuals with type 1 diabetes and chronic kidney disease.
We recently compared the number of glomeruli, i.e. nephrons in hypertensive adults and matched normotensive adults both of whom had been victims of traffic accidents. As shown in table 1 the number of glomeruli was significantly lower in hypertensive individuals, whilst the volume of glomeruli was significantly higher (”oligomeganephrony”).
Table 1. Keller, New Engl J Med (2003) 348: 101.
This finding immediately raises an issue: in individuals with reduced nephrons following alive kidney donation no excess frequency of hypertension is observed and at best a minor increase of blood pressure was found in a large metanalysis. This observation is in line for instance with the 25 year follow up after uninephrectomy of American servicemen in World War 2 where Narkun-Burgess failed to see an excess of high blood pressure. This is in striking contrast with what is found experimentally following uninephrectomy after birth and with what is observed in young individuals with reduced nephron numbers as a result of congenital malformation. In 157 patients with unilateral agenesis and normal contralateral kidney Argueso found that 7% had high blood pressure; 13% reduced renal function and by age 37 years 6 individuals out of 157 had already succumbed to renal failure.
In the study of Keller we found less glomeruli of larger size; if one calculates an index of the glomerular surface area, however, the surface available for filtration remains within the normal range. Obviously developmental changes in postglomerular segments must account for high blood pressure; various postglomerular mechanisms have been identified such as upregulation of sodium channels, upregulation of angiotensin receptors, activation of the mineralcorticoid receptor by diminution of the activity of 11-beta hydroxysteroid-dehydrogenase 2, sympathetic overactivity and others.
The assumption that increased tubular sodium reabsorption plays a role is strengthened by the observation of De Boer that low birth weight is associated with salt sensitivity of blood pressure in healthy adults.
These studies mentioned addressed Caucasoids. Interestingly in hypertensive blacks no reduction of glomerular number is found. Furthermore Rostand noted no correlation between low birth weight and higher blood pressure in blacks, although this correlation was clearly demonstrated in whites.
It should also be noted that one factor raising the risk of a higher blood pressure in the offspring is maternal smoking during pregnancy; even in early childhood at age 3 a significant association was found between systolic blood pressure of the child and a smoking history of the mother – this was independent of birth weight.
Low birth weight and the risk of albuminuria, chronic kidney disease and endstage renal disease
A Norwegian study noted that individuals with low birth weight had a greater risk to undergo kidney biopsy in adult age during their lifetime, consistent with increased predisposition to develop renal problems attributable to low birth weight.
It is also known that primary kidney diseases progress faster in individuals with a history of low birth weight, as shown for the nephrotic syndrome or IgA glomerulonephritis.
A recent study documented a relation between birth weight and the prevalence of different stages of chronic kidney disease: compared to matched controls with a birth weight of 3.46±0.6 kg, the birth weight in CKD patients was significantly lower (3.27±0.6 kg). It has been shown that low birth weight is associated with a higher risk of CKD at least in males (not in females presumably because of lower overall renal risk). This year Vikse showed that children born in Norway 1967-2004 with a birth weight below the 10th percentile had a 50% higher adjusted relative risk to experience endstage renal disease. This is presumably even an underestimation because in these individuals up to age 30 the general risk of CKD is low, but the risk will presumably further increase with advancing age.
The notion that a low complement of nephrons at young age predisposes to hypertension and chronic kidney disease later in life is well supported by experimental evidence. Woods uninephrectomized SD-rats and exposed them at age 8 and 20 weeks to low or high salt diet. On high salt she noted higher protein excretion and histological evidence of glomerular damage as well as salt sensitivity of blood pressure progressing in intensity from the 8th to the 20th week of age. A reduced number of glomeruli after uninephrectomy also sensitizes the kidney to superimposed injury. Miller infused angiotensin II (50 ?g/minute) or saline in uninephrectomized rats. Angiotensin II infusion caused more prominent albuminuria and more severe glomerulosclerosis compared to sham-operated rats.
Prenatal Programming and Metabolic Syndrome
In agreement with a substantial body of experimental evidence it has been shown in several studies, for instance by Bhargava, that individuals who develop impaired glucose tolerance or type 2 diabetes are born with a lower body mass index. Later on in life, however, they experience catch up growth and adult obesity. A similar evolution is seen not only for diabetes, but also for cardiovascular events: Barker studied women who experienced myocardial infarction at approximately 40 years of age. Their birth weight had on average a Z-score lower by 0.2; at an age of approximately 6 years the Z-score had crossed the line indicating progression to high body weight.
We therefore propose the hypothesis (fig. 1) that prenatal programming is one of the factors that link the cardiovascular and renal risk at adult age. Disturbed prenatal programming exposes the kidney to the risk of nephron underdosing; this in and by itself is presumably not sufficient to cause chronic kidney disease, but sensitizes the kidney to second hits such as the occurrence of IgA glomerulonephritis, diabetic nephropathy and others which then evolve more rapidly to macroproteinuria, rapid loss of GFR and endstage kidney disease. The parallel sequence of increased cardiovascular and renal risks could explain, at least in part, why the cardiovascular risk is so excessively high in renal patients.
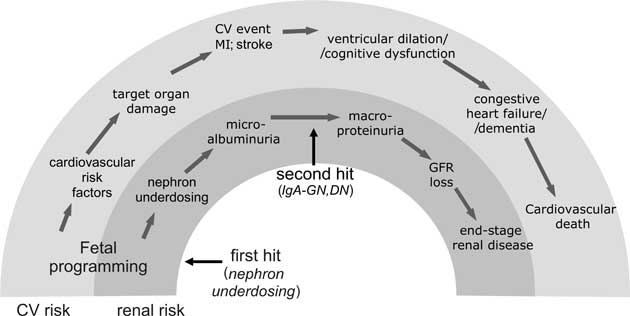 Fig. 1. Prenatal programming – link of adult cardiovascular and renal risk.
A brief comment on one specific risk factor namely maternal hyperglycemia; high glucose concentrations during pregnancy (diabetes of pregnancy) increases not only the risk of type 2 diabetes and the cardiovascular risk in the offspring, but also amplifies his or her renal risk. As shown in table 2 when streptocotozin diabetes is produced in pregnant rats with either low or high degrees of hyperglycemia, the kidney weight in the offspring is reduced as is the number of glomeruli. Interestingly not only maternal hyperglycemia, but also maternal hyperinsulinemia provokes adverse effects in the offspring. Bursztyn showed that the offspring of dams with maternal hyperinsulinemia developed higher blood pressures later in life.
Table 2. Less nephrons in offspring of diabetic rats. Amri, Diabetes (1999) 48: 2240.
A link between maternal glycemia and renal risk is illustrated by an observation in Pima Indians by Nelson. He studied the prevalence of albuminuria in offspring of pre-diabetic mothers who had been normoglycemic during gestation and mothers who had been hyperglycaemic during gestation. Both groups of mothers had the same genetic risk of type 2 diabetes prevailing in the Pima Indian tribe – yet 40% of the offspring of pre-diabetic mothers with normoglycemia during pregnancy had albuminuria, compared to 70% of the offspring of diabetic mothers with hyperglycemia during pregnancy.
The above incomplete listing of the available evidence clearly documents data that intrauterine pathology exerts a powerful influence on different pathologies later in adult life.
**Dedicated to Franciszek Kokot – a long standing friend and inspiring scientist.
Piśmiennictwo
1. Kermack WO, McKendrick AG, McKinlay PL: Death-rates in Great Britain and Sweden: some general regularities and their significance. Lancet 1934; i: 698.
2. Barker DJ et al.: Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ 1989; 298(6673): 564-567.
3. Brenner BM, Garcia DL, Anderson S: Glomeruli and blood pressure. Less of one, more the other? Am J Hypertens 1988; 1(4 Pt 1): 335-347.
4. Gluckman PD et al.: Effect of in utero and early-life conditions on adult health and disease. N Engl J Med 2008; 359(1): 61-73.
5. Woods LL et al.: Maternal protein restriction suppresses the newborn renin-angiotensin system and programs adult hypertension in rats. Pediatr Res 2001; 49(4): 460-467.
6. Wlodek ME et al.: Growth restriction before or after birth reduces nephron number and increases blood pressure in male rats. Kidney Int 2008; 74(2): 187-195.
7. Amri K et al.: Altered nephrogenesis due to maternal diabetes is associated with increased expression of IGF-II/mannose-6-phosphate receptor in the fetal kidney. Diabetes. 2001; 50(5): 1069-1075.
8. Bursztyn M et al.: Adult hypertension in intrauterine growth-restricted offspring of hyperinsulinemic rats: evidence of subtle renal damage. Hypertension 2006; 48(4): 717-723.
9. Balbi AP, Costa RS, Coimbra TM: Postnatal renal development of rats from mothers that received increased sodium intake. Pediatr Nephrol 2004; 19(11): 1212-1218.
10. Woods LL, Weeks DA: Prenatal programming of adult blood pressure: role of maternal corticosteroids. Am J Physiol Regul Integr Comp Physiol 2005; 289(4): R955-962.
11. Manalich R et al.: Relationship between weight at birth and the number and size of renal glomeruli in humans: a histomorphometric study. Kidney Int 2000; 58(2): 770-773.
12. Silver LE et al.: Intrauterine growth restriction is accompanied by decreased renal volume in the human fetus. Am J Obstet Gynecol 2003; 188(5): 1320-1325.
13. Spencer J, Wang Z, Hoy W: Low birth weight and reduced renal volume in Aboriginal children. Am J Kidney Dis 2001; 37(5): 915-920.
14. Konje JC et al.: A cross-sectional study of changes in fetal renal size with gestation in appropriate- and small-for-gestational-age fetuses. Ultrasound Obstet Gynecol 1997; 10(1): 22-26.
15. Uiterwaal CS et al.: Birth weight, growth, and blood pressure: an annual follow-up study of children aged 5 through 21 years. Hypertension 1997; 30(2 Pt 1): 267-271.
16. Horta BL et al.: Early and late growth and blood pressure in adolescence. J Epidemiol Community Health 2003; 57(3): 226-230.
17. Fagerudd J et al.: Birth weight is inversely correlated to adult systolic blood pressure and pulse pressure in type 1 diabetes. Hypertension 2004; 44(6): 832-837.
18. Keller G et al.: Nephron number in patients with primary hypertension. N Engl J Med 2003; 348(2): 101-108.
19. Fehrman-Ekholm I et al.: No evidence of accelerated loss of kidney function in living kidney donors: results from a cross-sectional follow-up. Transplantation 2001; 72(3): 444-449.
20. Boudville N et al.: Meta-analysis: risk for hypertension in living kidney donors. Ann Intern Med 2006; 145(3): 185-196.
21. Narkun-Burgess DM et al.: Forty-five year follow-up after uninephrectomy. Kidney Int 1993; 43(5): 1110-1115.
22. Woods LL, Weeks DA, Rasch R: Hypertension after neonatal uninephrectomy in rats precedes glomerular damage. Hypertension 2001; 38(3): 337-342.
23. Mei-Zahav M et al.: Ambulatory blood pressure monitoring in children with a solitary kidney – a comparison between unilateral renal agenesis and uninephrectomy. Blood Press Monit 2001; 6(5): 263-267.
24. Argueso LR et al.: Prognosis of patients with unilateral renal agenesis. Pediatr Nephrol 1992; 6(5): 412-416.
25. de Boer MP et al.: Birth weight relates to salt sensitivity of blood pressure in healthy adults. Hypertension 2008; 51(4): 928-932.
26. Hughson MD et al.: Hypertension, glomerular number, and birth weight in African Americans and white subjects in the southeastern United States. Kidney Int 2006; 69(4): 671-678.
27. Rostand SG, Cliver SP, Goldenberg RL: Racial disparities in the association of foetal growth retardation to childhood blood pressure. Nephrol Dial Transplant 2005; 20(8): 1592-1597.
28. Blake KV et al.: Maternal cigarette smoking during pregnancy, low birth weight and subsequent blood pressure in early childhood. Early Hum Dev 2000; 57(2): 137-147.
29. Vikse BE et al.: Adverse perinatal outcome and later kidney biopsy in the mother. J Am Soc Nephrol 2006; 17(3): 837-845.
30. Na YW et al.: Effect of intrauterine growth retardation on the progression of nephrotic syndrome. Am J Nephrol 2002; 22 (5-6): 463-467.
31. Zidar N et al.: Effect of intrauterine growth retardation on the clinical course and prognosis of IgA glomerulonephritis in children. Nephron 1998; 79(1): 28-32.
32. Al Salmi I et al.: Birth weight and stages of CKD: a case-control study in an Australian population. Am J Kidney Dis 2008; 52(6): 1070-1078.
33. Li S et al.: Low birth weight is associated with chronic kidney disease only in men. Kidney Int 2008; 73(5): 637-642.
34. Vikse BE et al.: Low birth weight increases risk for end-stage renal disease. J Am Soc Nephrol 2008; 19(1): 151-157.
35. Miller PL, Rennke HG, Meyer TW: Glomerular hypertrophy accelerates hypertensive glomerular injury in rats. Am J Physiol 1991; 261(3 Pt 2): F459-465.
36. Bhargava SK et al.: Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med 2004; 350(9): 865-875.
37. Barker DJ et al.: Trajectories of growth among children who have coronary events as adults. N Engl J Med 2005; 353(17): 1802-1809.
38. Amri K et al.: Adverse effects of hyperglycemia on kidney development in rats: in vivo and in vitro studies. Diabetes 1999; 48(11): 2240-2245.
39. Nelson RG, Morgenstern H, Bennett PH: Intrauterine diabetes exposure and the risk of renal disease in diabetic Pima Indians. Diabetes 1998; 47(9): 1489-1493.
otrzymano/received: 2009-07-17 zaakceptowano/accepted: 2009-09-02 Adres/address: *Eberhard Ritz Ruperto-Carola University Nierenzentrum Im Neuenheimer Feld 162, D-69120 Heidelberg, Germany tel.: +48 0049-6221-601705 e-mail: Prof.E.Ritz@t-online.de Pełna wersja artykułu Prenatal Programming – impact on the kidney and beyond** dostępna w Czytelni Medycznej Borgis. |
Chcesz być na bieżąco? Polub nas na Facebooku: strona Wydawnictwa na Facebooku |








