|
© Borgis - Postępy Nauk Medycznych 9, s. 678-684
*Katarzyna Osiak, Józef Jethon
Surgical treatment of rhinophyma
Chirurgiczne leczenie guzowatości nosa
Medical Centre of Postgraduate Education, Department of Plastic Surgery
Professor W. Orłowski Hospital Head of the Department: prof. Józef Jethon, M.D. Streszczenie
Rhinophyma it is the latest phase of acne rosacea. The development of an enlarged, red bulbous nose was once thought to be caused by heavy alcohol consumption, but this is not the case. Rhinophyma occurs equally in those who do not drink at all and those who drink alcohol excessively. Rhinophyma typically afflicts white males between 40 and 60 years of age. It is 12 times more common in men than women. It begins with rosacea which progresses to acne rosacea. It is more severe form of acne rosacea. With time, the vessels of the nose become progressively dilated. Multiple cysts and pustules grow in the thickened oily skin. As sebaceous glands become more and more hypertrophied, the nasal tip widens. As the deformity worsens, pits, nodules, fissures, lobulations and pedunculations distort the nose into a grotesque organ. Histopathologically there is hyperplasia and hypertrophy of the sebaceous glands, and the ducts become elongated, dilated, and plugged. There is irregular fibrous tissue proliferation with varying degrees of inflammatory cell infiltration. Foreign body reactions are not unusual. Nonsurgical treatment is similar to acne: meticulous cleaning, skin hygiene. Avoidance of food that seem to worsen the condition. Antibiotics may be useful when small infections are present. Surgical treatment consists of dermaplanning and dermabrasion. Laser treatments can also be used, but can be harder to control the depth of injury. In this condition the pores of the skin go very deep. Regrowth of skin comes from these deeper skin elements. Surgery is usually performed under local anesthesia as an outpatient. The raw skin after surgery can drain and needs careful care not to damage the remaining skin elements. The speed of healing depends on many factors such as the depth of surgery and your own healing tendencies. The authors show their own experience in surgical treatment of 18 rhinophyma patients with good esthetic results. Słowa kluczowe: rhinophyma, acne rosacea, soft-tissue hypertrophy of the nose, surgical treatment
Summary
Guzowatość nosa jest końcową fazą trądziku różowatego, która dotyka prawie wyłącznie pacjentów płci męskiej i charakteryzuje się postępującą deformacją kształtu nosa. Za jedną z przyczyn powstawania tego zniekształcenia uważano nadmierne spożycie alkoholu, co nie zostało potwierdzone. Zmiany chorobowe rozwijają się najczęściej u mężczyzn pomiędzy 40. a 60. rokiem życia. Guzowatość nosa 12 razy częściej występuje u mężczyzn niż u kobiet. Na podłożu zmian trądzikowych z wiekiem rozwija się trądzik różowaty. Z czasem dochodzi do rozszerzenia naczyń krwionośnych nosa i rozwoju mnogich torbieli łojowych i drobnych ropni w pogrubiałej i łojotokowej skórze. Wraz z poszerzaniem się gruczołów łojowych dochodzi do poszerzenia i zniekształcenia zarysu czubka nosa. W zależności od stopnia deformacji guzowatość nosa może zniekształcać wygląd dotkniętych nią chorych i przez to mogą się oni stać upośledzeni pod względem psychospołecznym. Zmiany histopatologiczne to przerost i rozrost gruczołów łojowych oraz wydłużenie i poszerzenie ich przewodów. Obserwuje się nieregularny rozrost tkanki łącznej włóknistej z naciekami komórek zapalenia o różnym nasileniu lub pojawieniem się komórek o typie wokół ciała obcego. Nieoperacyjne metody leczenia trądziku różowatego są podobne do leczenia zwykłego trądziku i obejmują utrzymanie higieny, oczyszczanie skóry oraz unikanie spożywania pokarmów zaostrzających stan zapalny w obrębie zmian. Farmakologiczne metody leczenia trądziku różowatego (antybiotykoterapia) mają zastosowanie we wczesnym okresie choroby. W zaawansowanej guzowatości nosa metodą przyjętą jest leczenie operacyjne. Leczenie chirurgiczne polega na stycznym ścięciu zmian chorobowych i dermabrazji. Leczenie laserem jest trudniejsze ze względu na trudności w ocenie głębokości zmian chorobowych. Do zagojenia rany dochodzi poprzez naskórkowanie z najgłębiej położonych i zachowanych części poszerzonych gruczołów łojowych. Zabiegi chirurgiczne wykonywane są zazwyczaj w znieczuleniu miejscowym w ramach chirurgii jednego dnia. Po zabiegu operacyjnym przez kilka pierwszych dni obserwuje się obfitą wydzielinę z rany. Podczas zmiany opatrunków zaleca się delikatne obchodzenie się z raną, aby nie uszkodzić pozostawionych elementów skory. Szybkość gojenia się rany zależy od wielu czynników takich jak głębokość cięcia chirurgicznego oraz osobnicze skłonności. Autorzy przedstawiają wyniki leczenia chirugicznego18 pacjentów w zaawansowanym stadium guzowatości nosa. Wyniki końcowe leczenia operacyjnego u wszystkich pacjentów uznano za dobre. 17 pacjentów zagoiło się samoistnie w ciągu 6-8 tyg. U jednego zaszła konieczność położenia przeszczepów skóry w związku z przedłużającym się gojeniem rany. Wszyscy pacjenci uznali końcowy efekt estetyczny za dobry lub bardzo dobry. Key words: rhinophyma, guzowatość nosa, trądzik różowaty, przerost tkanek miękkich nosa, leczenie operacyjne
Introduction
The bulbous deformity of the nose, called rhinophyma it is a disease known from years. The desciptive term was used for the first time by Ferdynand Hebra at 1845, from the Greek „rhis” meaning nose and „phyma” meaning growth (2). It was probably known to Greek and Arabian physicians as early as 2000 B.C. but it cannot be confirmed. In those early days there were several tuberous conditions of the nose such as tuberculosis, syphilis and leprosy which were likely confused with rhinophyma. The medical literature is silent for centuries, but the condition is well documented in art and literature. The old man from the famous XV century painting of the Rafael Santi teacher, Domenico Ghirlandaio titled „The Old Man and his Grandson” has his nose distinctively and characteristically deformated (fig. 1).
 Fig. 1. Portrait of an Old man with a Young Boy Wood (http://przeslanie.nd.e-wro.pl/wkamin3/galeria/girlandaio%20and%20gris/stary%20czlowiek.html).
Rhinophyma it is the end-stage of acne rosacea. It is a disease leading to irregular growth of soft tissues of the external nose, with severe deformation of a tip and wings of a nose. It typically afflicts white males between 40 and 60 years of age, although there have been a few patients who developed it in their 20 s. It is far more common in men than I women, with the ratio of 12:1 generally reported. This is very interesting when you consider that the disease is the end stage of acne rosacea, which is three times more common in females. It is slightly present in black race. This epidemiological data underline the importance of genetic factors- not yet identified – but they don´t help to understand the real etiology of this disease, which still remains unknown. One study by Freeman et al in 1970 reported that 12 of 55 patients had parents or grandparents with similar nasal disfigurements.
In the past the rhinophyma was considered a clinical sign of alcoholism, but this relationship was never demonstrated. Ethiopatogenesis of this disease in finally unclear and unknown. In the same way is unclear the correlation between a steroid hormones excessive effect and the hypertrophy of sebaceous glands, which is peculiar of rhinophyma, or between rhinophyma and some microorganisms, like the Demodex Foliculorum, often isolated in this disease. Common and early characteristic in the etiology of acne rosacea is a recurrent and fleeting vasodilatation of the face that, according to Marsili and Cockerell would cause a soft – tissue nasal hypertrophy, gradually giving rise to rhinophyma.
It begins as an accentuation of the normal flush reaction an adolescence and young adulthood and can involve the nose, central forehead, malar areas, and chin. With time, the vessels of the nose become progressively dilated and the skin thickens and may become involved with cysts and pustules, and the skin can be quite oily. The nose thickens at the tip and sebaceous glands hypertrophy, as the deformity worsens, pits, nodules, fissures, lobulations, and pedunculation contort the nose into grotesque cosmetic problems. There is no uniformity in the end stage of final appearance. Progression of disease in the chin has been termed „mentophyma”, and involvement of the pinna can lead to otophyma”, but these areas are much less frequently involved than the nose. It may cause not only cause the face deformity, but also lead to some respiratory problem. The functional complaint involves a nasal airway obstruction as the mass remodels the nasal tip often producing total occlusion. It may cause some ophtalmic complications such as blepharitis, conjunctivitis, corneal erosion and iriditis.
Histopathologically there is hyperplasia and hypertrophy of the sebaceous glands and the ducts become elongated, dilated, and plugged. There is irregular fibrous tissue proliferation and varying degrees of inflammation with inflammatory cell infiltrate and bacteria seen. Foreign body reaction can be seen. In fact, the peculiar morphologic characteristics of rhinophyma are:
1. teleangiectasy,
2. hypervascularity,
3. a thick nasal cutaneous layer,
4. nodularity covered by atrophic skin with expanded pores.
According to this clinical data rhinophyma is classified in five forms (tab. 1).
Table 1. Rhinophyma – morbid stages, characteristics.
In the first stage there in moderate hypertrophy of blood vessels.
In the second stage massive hyperplasia of sebaceous glands, elastosis in the derma, moderate fibrousness with collagene fibers plugged in mixoid oedematous stroma, many follicular cysts and lympho histiocyte infiltration around expanded blood vessels are present.
In the third stage we can observe severe fibrotic alterations in the derma, decrease or lack of sebaceous glands and dermal adnexes.
In the fourth and fifth degree it is presence of tumorous changes In the and dilated sebaceous glands in the different parts of the nose, with dilated blood vessels over the whole surface of the nose.
Many have reported the presence of occult basal cell carcinomas in removed rhinomatous tissues in the range of 3% to 10% of cases, and Graham and McGavran (1964) have demonstrated that basal cell carcinomas occur in direct proportion to the concentration of sebaceous glands in sun exposed skin. Squamous cell carcinomas and other tumors have also been seen in an association that can only be considered incidencial.
Depending on the stage of rhinophyma, it may cause severe cosmetic deformity and influence on the psychosocial condition of the patient.
Treatment of rhinophyma
Medical treatment, when used, is usually undertaken before and in conjunction with surgical treatment. Acne rosacea may respond to local medical or dermatologic treatment and prevent progression to rhinophyma. Medical treatment classically has been limited to the avoidance of stimulation factors, appropriate clearliness, and treatment of secondary infection and inflammation with antibiotics and steroids. There have been many studies of treatment with vitamins, hormones, fibrinolysis, steroids, ice flush, liquid oxygen, liquid nitrogen, silver nitrate, caustic, mercury vapor, ultraviolet wave, and others, but none have been to be particular effective. More ancient remedies involving herbs, spices, potions were ineffective.
Modern topical therapy includes cleansing the skin with detergents that have defatting effects, avoiding creams or ointments. Anti-inflammatory and antibacterial medications in a non-irritating base or benzoyl peroxide (3-5%) are often helpful. Topical corticosteroids have no place in the treatment of rosacea. It is true that they can be effective over a short period, but the disease recurs after it is discontinued and long term use can lead to steroid-damaged skin. Weak concentrations of sulphur (2%), or icthyol (2%) may be helpful in some cases.
Systemic therapy includes oral antibiotics such as Metronidazole (Flagyl 250 mg/day x 10 days) for acute exacerbations. Long term use is contraindicated because of risk of polyneuropathies and possible carcinogenic effects. Tetracycline (250-500 mg/day can be used in more long-therm management but is often less effective. Isoretinoin (13-cis-retinoic acid-Acutane) in doses of 0.2-1.0 mg/kg for 10-16 weeks has been shown to provide to reduction in the volume of sebaceous glands (3).
Surgical treatment
Once the violaceous, hypertrophic, bulbous stage of the disease becomes manifest, only surgical manipulation can reverse the deformity. The partial thickness excision (tangential) it is the treatment of choice, is thermed decortications, and is recommended by most authors. The idea is that the rhinomatous tissue is shaved off in layers with care taken not to injure the underlying cartilage. The operator may place fingers in the nostrils or use magnification in order to halt removal of tissue once a thickness of 2-3 mm above the upper and lower lateral cartilages and nasal bones is estimated to remain. At this point the remaining fundi of the hypertrophic sebaceous glands should be sufficient to totally re-epitelialize the nose. If one stops resecting above this plane, the nose remains bulbous, and to go below it will leave raw granulating, non epithelializing areas. Areas that are difficult to mold and refine with the scalpel can be dermabraded to achieve a better result. Decortication retains the overall architecture of the nose and reformation of sebaceous gland pores contributes to a more normal surface texture. Additionaly, the color match of the re-epithelialized nose is closer to normal than any of the skin grafting techniques.
The tangential decortications of the nose can be performed using surgical scalpel, cryosurgical techniques, chemical peels, dermabrasion, the cold scalpel, the termally heated scalpel, the Bovie, hot wire loops, and the Argon and Co2 lasers. The scalpel and dermabrader often lead to significant bleeding. Electrosurgical techniques are better, but most authors recommend use of the CO2 laser which can allow operation in a bloodless field.
The depth of excision is determined by visualization of the nasal contour and by the distint crackling sound and odor emited by sebaceous elements exudes ribbons of sebaceous materials so that if you don´t see sebum or hear crackling, you are probably too deep. Particular care is taken around the nasal alae.
Wound care consists of covering with antibiotic-impregnated or other nonadherent gauze (e,g, Xeroform). The gauze is removed between the third and fifth postoperative day and antibiotic ointment application (bacitracin, neomycin) is continued until re-epithelialization occurs, which may take up to three or four weks.
Early complications include hemorrhage and wound infection. Exposure of cartilage can lead to chronic infection and chondronecrosis with resultant deformity, so that if the cartilage is exposed, it should be covered by grafting. This is particulatly true along the nasal alae where injury can lead to notching that may be particulatly difficult to correct.
Late complications include delayed healing which may lead to eschar formation and cicatrix. Most commonly, this occurs after decortications at a level just below the sebaceous elements. If the wound has failed to heal by three to four weeks postop, split thickness skin grafting should be carried out. Excessive scarring is best avoided by adhering to the above principles, paying attention to the depth of excision and avoiding exposure of cartilage. Irregular or prominent scars may sometimes be improved by dermabrasion. Color mishmatch from grafting may improve gradually, but is best avoided by careful preoperative planning (4).
Patients and methods
Authors present 18 consecutive patients that were treated because of rhinophyma at Plastic Surgery Clinic in the period of 2000-2009. Every patient was men, age 48-72 y, the period of deformity of the nose varied between 3-20 yrs (tab. 2).
Table 2. Surgical treatment of rhinophyma.
All were healthy. Three of them were alcohol abusers. Antibiotics (tetracycline) taken by 12 patient for years were noneffective. Two had received no preoperative antirosacea medication.
Patient were treated by surgical decortication of rhinophyma.
Surgical technique of rhinophyma
1. Outline the borders of the rhinophyma with normal tissue.
The peripheral margin is outlined demarcating normal from abnormal tissue
2. Draw vertical parallel lines (or only one central vertical line, depending on the size and shape of tumor), dividing the rhinophyma into arbitrary sections. The alar rims may be divided into three sections when indicated.
3. Local anaesthesia application.
Approximately 20-30 ml of 0.5% xylocaine with epinephrine 1/100 000 is forcibly infiltrated around and into the rhinomatous lesion expanding the nose. Significant pressure is required to inject this quantity of solution into rhinophyma. This compresses the vessels and affords a much dryer surgical field. It is required to wait 10-12 minutes and then slowly sgueeze out the edema of the nose over the gauze pad. The nose will be blanched, and of normal size.
4. Tangential excision.
With a number 15 scalpel blade score the entire margin of the rhinophyma at a shallow angle (~30°) to the skin surface. There should now be a miniscule amount of bleeding, because all large vessels are below the glandular rhinophyma layer. Neither cautery nor laser will be necessary.
With a number 10 blade excise the rectangles symmetrically left and right into the rhinophyma mass, leaving the open pores of the glands at the base as source of epithelialization. Accurate excision is not necessary at this point, but is important not to excise below the base of the cystic hypertophic sebaceous tissue, because this increases the potential of scarring. The surgeon may excise the hypertrophic of rhinophyma down to within 1 mm from the cystic base. This procedure may be accomplished in stages until the surgeon reaches a comfort level. The surgeon must accurately visualize the glands through the adjacent excised effect, because bleeding does not obstruct the view.
6. Dermabrasion.
After a bulk of all glandular tissue has been removed the tissues can be lightly dermabraded so the nose is symmetrical. Abrasion is done with medium – grit wheel or diamond fraise at relatively slow rotations per minute. A finger inserted inside the naris adds counter – support. Dermabrade toward the center of the defect superiorly and toward the nasal aperture inferiorly.
7. Haemostasis.
Do the careful haemostasis and put xeroform gauze over the nasal defect.
8. Management of the wound.
Clean the wound and peripheral tissues with 3% sol peroxide every day and then put 5% sol of KMnO4 directly on the wound.
9. Postoperative management.
The patient should be controlled every week in the outpatient clinic. After 1 month-6 weeks we can observe excellent wound healing. Sometimes we noted a small scar at the superior junction of normal skin to rhinophyma. The patients was delighted with the result and deffered the use of silicone sheeting or steroid injection into the small scar.
Intraoperative surgery entailed 1-1.25 hours in all cases. There was minimal intraoperative blood loss (always less than 5 cc), and no operative bleeding. The operative technique was tangential cut of tumorous tissues of rhinophyma. The depth of cut should be in the layer that left the bottoms of the glandulae. Patients did not require postoperative narcotic analgesics. Postoperative care was easily managed by the patient with verbal instructions. Scarring was minimal. Patient acceptance was excellent. The excellent haemosthasis was performed.
Results
Surgical treatment of rhinophyma allowed achieve a good sight and good cosmetic result in every patient. Spontaneous epithelialisation of the surgical wound was observed after 4-9 weeks.
One patient with monstrual overgrowth of the soft tissues of the nose was put free skin transplant to enable the wound healing. But the end cosmetic effect was good ant the shape and function of the nose was excellent.
In 5 cases the prolonged healing and hypertrophic scar was observed. These patients required silicone dressings management during the postoperative period.
Every patient were administered intravenous and oral antibiotics (Unasyn 3x750 mg/3 days at hospital and amoxicillin with clavulanian acid 2x1.0/7 days at home).
In one case the postop wound bleeding was observed on 2nd and 5th day after operation and the patient was admitted to the hospital again.
There was no correlation between the medical or dermatological treatment and surgical treatments results, wound healing time and hospitalization period.
Discussion
This article presents a limited, technique dependent surgical approach to rhinophyma. This procedure may be contemplated under sedation and local anesthesia.
The overall patient examination should include intranasal examination, and the potential of tumor in the rhinophyma tissue should be considered. All surgical specimens were sent to the pathology laboratory for permanent histologic evaluation.
Medical and dermatologic histories will often yield crucial information like the use of Retin A or Accutane which should have been discontinued for 6 to 12 months before surgical intervention.
The authors believe that definitive therapy for rhinophyma will ultimately become surgical. Inactive, uninflamed rhinophyma may be treated immediately. Acutely inflamed rhinophyma should be reduced with topical or oral antibiotic medications, eg tetracycline orally and metronidazole gel.
No significant pain has been reported after this surgery. Defect resolution has been acceptable cosmetically. As long as the tissue beneath the epidermal rhinophyma is not encroached upon during surgical excision, which could produce a full thickness skin defect, scarring should be minimal. Skin grafts over an excised rhinophyma base have been routinely unesthetic.
Dressing changes have been scheduled at once a day. No patient encountered any difficulty with home care. Antibiotics were administered orally for 7 days after surgery.
Nasal blanching
The old canard that solutions containing ephinephrine should not be injected into fingers, toes, ears nose and penis is refuted daily by surgeons who operate on ears and nose. The nose is almost white and does not bleed. Even after final absorption of the local anaesthesia in the recovery room and on the postoperative visits no rebleading has occurred in any patient. Nor has ever been any evidence of skin necrosis. Total blood loss did not exceed a guess-estimate of 5 cc, because there was a miniscule amount of bleeding during the excision, and minimal tissue spray or plume during the dermabrasion.
Painless surgery
The authors operate under local anaesthesia, and remarkably, no patient complained of any pain that necessitates narcotics postoperatively during the week of healing (7).
A case presentation
A 68 year-old-man with mild hypertention reduced from 10 years presented to the Plastic Surgery Department complaining of extremely big tumorous deformity of the nose over a 20 year period. He noted that changes in his skin began at age 20. He has been followed by Dermatology for many years, where he has received intermittent 1% hydrocortisone cream treatment and various antibiotics, most commonly tetracycline 250 mg orally on twice daily schedules. Over recent years he has noted nasal obstruction and the giant overgrow of his nasal tip. The tumor was so big that covered his upper lip and disabled normal feeding (fig. 2, 3).
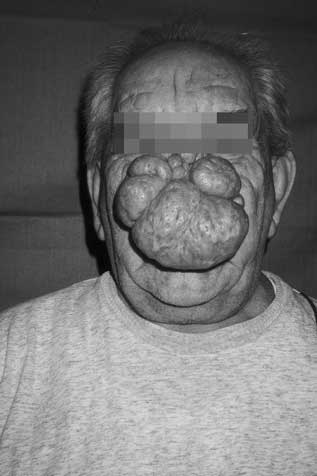 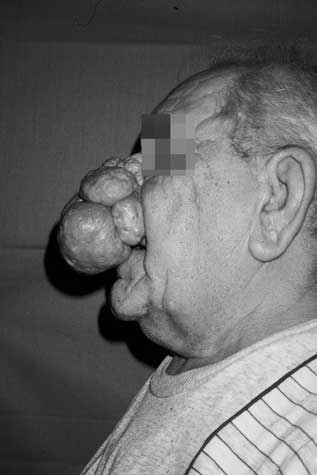 Fig. 2, 3. 68 year-old-man with extremaly big deformity of the nose (5th morbid stage) and nasal obstruction. Patient before the operation.
Patient was operated under local anesthesia with 0.5% xylocaine with epinephrine solutio. The operation was performed with 15 surgical blade. The bulky rhinophymatosus tissues were cut tangentially in the layer leaving the bottoms of glands. But in fact it was difficult to obtain the proper level because of extreme deformation of the dorsum and tip of the nose. The early perioperative period was uneventful. After a week the wound stopped draining and was covered by split thickness skin graft from the left tigh skin. The donor site were covered by Koch dressing (xeroform gauze with silicone and dry gauze).
The free split thickness skin graft was covered by silicone and xeroform gauze and gauze soaked with 3% boric acid solution. The skin transplant completely healed in 10 days period. The silicone dressing were not applied in this patient. The esthetic and functional effect was quite good. The shape and symmetry of the nose was perfect and no obstruction of the nose was present. The colour of the skin grafts was similar to surrounded skin (fig. 4, 5).
  Fig. 4, 5. Because of prolonged healing, the split thickness skin graft was applied 3 weeks after surgical procedure. Patient 6 weeks after operation.
Piśmiennictwo
1. Wyględowska-Kania M et al.: Skuteczność chirurgicznego leczenia przerosłej postaci trądziku różowatego rhinophyma. Dermatol Estetyczna 2002; 5: 2684.
2. Randall S Zane: MD-Rhinophyma 2001-2006 Baylor College of MedicineBobby R. alforg Department of Otolatyngology-Head and Neck Surgery http://www.bcm.edu/oto/grand/102992.html
3. Jordi Rex, Miguel Ribera, Isabel Bielsa: Postępowanie chirurgiczne w guzowatości nosa: doniesienie dotyczące ośmiu pacjentów
leczonych za pomocą elektrocięcia. Dermatologica 2005; 4: 58-62.
4. Mathes-Plastic Surgery: Epidermal Appendage Tumours second edition 2006; 5: 256-257.
5. Bermant M: Rhinophyma(Acne Roacea) – Bermant Plastic Surgery http://www.plasticsurgery4u.com/procedure_folder/rhinophyma_folder/rhinop.
6. Borzęcki A, Cielica W, Łoza K: Guzowatość nosa – leczenie laserem CO2. Doświadczenia własne. Nowa Medycyna, nr 1/2003 http://www.ctl.com.pl/art/art6.html
7. Zide M: Surgical Removal of Rihinophyma. Journal of Oral and Maxillofacial Surgery 2008; 66, 10: 2168-2177.
otrzymano/received: 2009-05-21 zaakceptowano/accepted: 2009-08-12 Adres/address: *Katarzyna Osiak Jesionowa Str. 39, 05-540 Zalesie Górne tel.: (0-22) 756-59-06 e-mail: kateosiak@gmail.com Pełna wersja artykułu Surgical treatment of rhinophyma dostępna w Czytelni Medycznej Borgis. |
Chcesz być na bieżąco? Polub nas na Facebooku: strona Wydawnictwa na Facebooku |








