|
© Borgis - Postępy Nauk Medycznych 6, s. 461-464
Barbara Polaczek-Krupa, *Iwona Grabska-Liberek
Use of retinal thickness analyzer (RTA) in diagnostics of diabetic macular edema1)
Zastosowanie analizatora grubości siatkówki RTA ( retinal thickness analyzer) w diagnostyce cukrzycowego obrzęku plamki
Department of Ophthalmology of the Medical Center of Postgraduate Education, Warsaw
Head of the Department: dr hab. med. sci. Iwona Grabska-Liberek Streszczenie
Introduction:The aim of the study is the evaluation of the retinal thickness in the macular region in diabetic patients with various stages of retinopathy by using the RTA analyzer and the assessment of applicability of this method in diagnosis of diabetic macular edema. Material and method: Forty diabetic patients (68 eyes) underwent full ophthalmologic examination and also retinal thickness analysis with an RTA analyzer. In particular, foveal average thickness FAV and posterior pole average thickness PPAV were determined. The data were statistically evaluated and compared with the data for a control group consisting of 80 sound voluntary persons (155 eyes). Results: Both FAV and PPAV values in the studied population of diabetic patients were significantly thicker than in the control group. Conclusions: The eyes with diabetic retinopathy can be examined by an objective method, like RTA, to diagnose the increased retinal thickness. The method can be recommended for screening the macular edema in diabetic patients because of its non-invasiveness, simplicity of the examination and further data evaluation. Słowa kluczowe: diabetes, macular edema, retinal thickness, retinal thickness analyzer, RTA
Summary
Wstęp:Celem pracy jest ocena grubości siatkówki w okolicy plamki u pacjentów z różnym stopniem zaawansowania retinopatii cukrzycowej przy pomocy analizatora grubości siatkówki RTA oraz ocena przydatności pomiaru grubości siatkówki w diagnostyce cukrzycowego obrzęku plamki. Materiał i metody: Czterdziestu pacjentów (68 oczu) z cukrzycą poddano szczegółowemu badaniu okulistycznemu oraz badaniu grubości siatkówki w okolicy plamki przy pomocy analizatora grubości siatkówki RTA. Badanie to obejmowało oznaczenie średniej grubości siatkówki w dołku FAV oraz średniej grubości siatkówki w tylnym biegunie PPAV. Otrzymane wartości liczbowe oceniono przy pomocy analizy statystycznej, porównując je z wartościami uzyskanymi dla grupy kontrolnej, obejmującej 80 zdrowych ochotników (155 oczu). Wyniki: Stwierdzono, że w grupie pacjentów z cukrzycą siatkówka w okolicy dołka i w okolicy tylnego bieguna jest znamiennie grubsza niż w grupie kontrolnej. Wnioski: Oczy z retinopatią cukrzycową mogą być przebadane przy pomocy obiektywnej metody pomiarowej, takiej jak analiza grubości siatkówki RTA, w celu wykazania możliwego pogrubienia siatkówki oraz rozpoznania obrzęku plamki. Wydaje się, że metoda ta może znaleźć szerokie zastosowanie w przesiewowych badaniach w kierunku obrzęku plamki u pacjentów z cukrzycą, ze względu na nieinwazyjność badania, prostotę obsługi urządzenia oraz łatwość oceny wyników badań. Key words: cukrzyca, obrzęk plamki, grubość siatkówki, analizator grubości siatkówki, RTA
Introduction
Diabetic retinopathy is responsible for many retinal changes observed in long-term diabetes. The permanent increase in the morbidity and the prolonged life time of the diabetics result in an increased occurrence of ophthalmic complications leading to irreversible blindness in developed countries.
The diabetic changes in blood vessels consist in thickening the basement membrane of capillaries, damage and proliferation of the capillary endothelial cells and loss of pericytes. The abnormalities contribute to the occlusion of small retinal vessels and to the reduction of the perfusion in the capillaries. The resulting retinal ischaemia and hypoxia lead to the formation of arteriovenous shunts, intraretinal microvascular abnormalities and leakage through the damaged vessel walls as well as localized and diffused retinal edema. The development of diabetic retinopathy results in formation of hemorrhages, microaneurysms, hard exudates, multiple cotton wool spots, neovascularization of retinal vessels, vascular-fibrous proliferations to the vitreous corpus and retinal detachment.
The most frequent reason for the blindness in diabetic patients is maculopathy consisting in retinal edema or hard exudates observed in the foveal region. In the case of clinically significant retinal edema, the treatment consists in photocoagulation of leakage sites with argon laser and resorption of the exudate. The good visual acuity can be retained after the treatment of the patient (1, 2).
Evaluation of retina by using the contact lens biomicroscopy at the dilated pupil is the basic clinical method of detecting of the macular edema. The efficiency of the evaluation depends, however, on the experience of the physician as well as on the macular edema extension. The blood vessel status and the extent of the leakages in the macula region can be evaluated by using fluorescein angiography (3). This method also allows to qualify diabetic patients to the laser coagulation treatment. The optical coherent tomography is also useful in evidencing the morphological changes of retina in diabetes.
The retinal thickness analyzer (RTA) seems also to be a good tool for the screening investigations. It enables a non-invasive examination of the retinal thickness in macula and it makes possible to identify the macular edema in the early stage of the disease (4, 5).
Purpose
The aim of the study was to evaluate the retina thickness in the macular region in diabetic patients on various stages of retinopathy by using the RTA analyzer and an assessment of applicability of the RTA method in diagnosis of diabetic macular edema.
Material
Sixty-eight eyes of 40 diabetic patients treated in the CMKP Department of Ophthalmology in 2005-2008 were included into the studied population. All patients underwent a detailed investigation, consisting of determination of visual acuity, intraocular pressure (applanation Goldmann tonometer) and lens transparency as well as evaluation of the fundus with Volk contact lens after pupil dilatation with tropicamide (1% solution). Patients with advanced hypertension, thyroid hyperactivity, pseudophakia and other eye surgery, retinal vein occlusion, advanced glaucoma and retina degeneration were excluded from the study. The eyes with lens and cornea opacity, low visual acuity and difficulties with the pupil dilatation were also excluded. The studied population was presented in the table 1.
Table 1. The studied population.
SD standard deviattion.
The diabetic retinopathy was classified according to the recommendations of the Research Group of Examination and Early Treatment of Diabetic Retinopathy (6). Both patients without any changes in the retina, patients with nonproliferative minimum and mild retinopathy (without any visible macular edema) and patients with visible macular edema were included in the studied population. The patients with visible macular edema underwent fluorescein angiography with Heidelberg Retina Angiograph HRA (Heidelberg Engineering, Germany).
Eighty healthy subjects (155 eyes) free of systemic and ocular diseases were in the control group. They appeared in the CMKP outpatient clinic for prophylaxis or getting glasses. The group was described in other paper (7) in detail. In the group, the retinal thickness did depended neither on patients´ sex nor on age.
Methods
The retinal thickness analysis was carried out with a non-invasive RTA analyzer (Talia Technology Ltd., Israel). The principle of the RTA is based on projecting a thin helium-neon laser slit through the dilated pupil obliquely on the retina and viewing it at an angle in a manner similar to slit lamp biomicroscopy. The separation between the reflections and scatter from the vitreoretinal interface and the chorioretinal interface is a measure of the retinal thickness. As the result, colored maps of the retinal thickness, graphs and respective numerical data were obtained (4). In particular, foveal average thickness FAV (area of 600 μm radius from fixation point) and posterior pole average thickness PPAV (area 6x6 mm excluding fovea) were determined both in the studied population and in the control group. The data were statistically evaluated and compared with the data of the control group (8, 9). The significance of differences between the average FAV and PFAV values in both groups was checked by Student t test.
A permission of the CMKP Bioethical Commission, Warsaw, was received (resolutions of 2nd March 2005 and 30th January 2008). Although no invasive methods were used in the study, the patients were fully informed of the aim and course of the study and they agreed.
Results
The results of the study were collected in the table 2. Both FAV and PPAV values in the studied population of diabetic patients were significantly thicker than those in the control group.
Table 2. Average FAV and PPAV values in the studied population.
*Difference highly significant (on the level 99.99%).
SD standard deviation. Discussion
An early detection of the macular edema is very important for taking the decision on fast treatment with laser coagulation and decreasing the risk of visual loss. The clinical evaluation of macular edema with biomicroscopy is supported with fluorescein angiography. This method can evidence the leakage from abnormal retinal blood vessels, however, does bring neither any information about degree of the fluid accumulation on the retina nor on the edema formation rate. At the first stage, no fluid accumulation in retina can take place at the normal absorption of the exudate. During the progress of the diabetic retinopathy, the exudate fluid is, however, accumulated in the retina what results in edema and in an increase of retinal thickness in macular region (3, 5, 10, 11). The fluorescein angiography has not any quantitative character and does not allow estimating the exudate fluid accumulation in the retina. Moreover, the angiography is an invasive method (fluorescein injection). Use of the RTA for an objective determination of the retinal thickness gives numerical data on the edema size and localization and its distance from the fovea (11, 12). Retinal thickness maps of healthy patients show a specific shape of the macula. It has C-shaped thickening above, below and nasally to the fovea. The analog maps for diabetic patients do not show any characteristic configuration in the foveal and perifoveal regions but evidence a thickening of retina in the studied area (fig. 1, fig. 2).
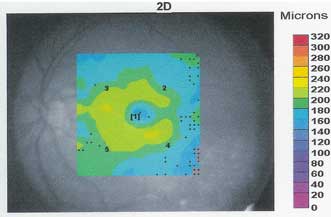 Fig. 1. Standard retina thickness map in a healthy subject.
 Fig. 2. Standard retina thickness map in a diabetic patient.
An increased thickness of retina in macular region in diabetic patients was described in many papers based on RTA and OCT methods (11, 13, 14, 15, 16). Our RTA studies showed a significant difference in the retinal thickness between the healthy and diabetic subjects and confirm our former observations (17). The observed increase in retinal thickness in diabetic patients can be assumed as subclinic and clinic symptoms of the macular edema and the measurement of the retinal thickness may be used for the diagnostic purposes.
Conclusions
The eyes with minimum and mild nonproliferative diabetic retinopathy without any visible macular edema should be examined by some independent objective methods, like RTA, to establish the increased retinal thickness in its initial stage. The method allows improving the accuracy of diabetic edema diagnosis, more frequent monitoring and an early start of the treatment in reduced area. The method is not widely used in Poland yet, but it can be recommended especially for screening the macular edema in diabetic patients because of its non-invasiveness, simplicity of the examination and further data evaluation.
1)The study was financially supported as CMKP projects No. 501-2-1-14-35/05 and No. 501-2-1-14-54/08.
Piśmiennictwo
1. Kański JJ, Milewski SA: Choroby plamki. Wrocław: Górnicki Wyd. Medyczne 2003.
2. Pecold K (ed.): Siatkówka i ciało szkliste. Wrocław: Elsevier Urban & Partner 2007.
3. Kałużny J, Mierzejewski A, Milewski S: Badania angiograficzne dna oka. Wrocław: Volumed 1998; 141-158.
4. Zeimer R et al.: A new method for rapid mapping of the retinal thickness at the posterior pole. Invest Ophthalmol Vis Sci 1996; 37: 1994-2001.
5. Asrani S et al.: Application of rapid scanning retinal thickness analysis in retinal diseases. Opthalmol 1997; 104: 1145-51.
6. Fong DS, Ferris FL: Postępowanie praktyczne w retinopatii cukrzycowej. Focal Points Ed Polska 2003; 21: 1-20.
7. Polaczek-Krupa B, Grabska-Liberek I: Ocena grubości siatkówki w okolicy plamki w populacji osób zdrowych przy użyciu analizatora grubości siatkówki RTA. Klinika Oczna, in press.
8. Moczko JA, Bręborowicz GH, Tadeusiewicz R: Statystyka w badaniach medycznych. Warszawa: Springer PWN 1998.
9. Petrie A, Sabin C: Statystyka medyczna w zarysie. Warszawa: Wyd. Lekarskie PZWL 2006.
10. Gieser JP et al.: Clinical assessment of the macula by retinal topography and thickness mapping. Am J Ophthalmol 1997; 124: 648-660.
11. Shahidi M et al.: Retinal thickness analysis for quantitative assessment of diabetic macular edema. Arch Ophthalmol 1991; 109: 1115-19.
12. Neubauer AS et al.: Tele-screening for diabetic retinopathy with the retinal thickness analyzer. Diabetes Care 2003; 26: 2890-7.
13. Pires I et al.: Retinal thickness in eyes with mild nonproliferative retinopathy in patients with type 2 diabetes mellitus. Comparison of measurements obtained by retinal thickness analysis and optical coherence tomography. Arch Ophthalmol 2002; 120: 1301-6.
14. Goebel W, Franke R: Retinal thickness in diabetic retinopathy: comparison of optical coherence tomography, the retinal thickness analyzer and fundus photography. Retina 2006; 26: 49-57.
15. Guan K, Hudson C, Flanagan JG: Comparison of Heildelberg retina tomography II and retinal thickness analyzer in the assessment of diabetic macular edema. Invest Ophthalmol Vis Sci 2004; 45: 610-6.
16. Fritsche P et al.: Retinal thickness analysis (RTA): an objective method to assess and quantify the retinal thickness in healthy controls and in diabetics without diabetic retinopathy. Retina 2002; 22: 768-71.
17. Polaczek-Krupa B, Grabska-Liberek I, Terelak-Borys B: Ocena grubości siatkówki w plamce u pacjentów z cukrzycą przy użyciu analizatora RTA. Klinika Oczna, in press.
otrzymano/received: 2009-04-08 zaakceptowano/accepted: 2009-05-06 Adres/address: * Iwona Grabska-Liberek Klinika Okulistyki CMKP ul. Czerniakowska 231, 00-416 Warszawa tel.: (0-22) 584-11-85 e-mail: k.okulistyki@szpital-orlowskiego.pl Pełna wersja artykułu Use of retinal thickness analyzer (RTA) in diagnostics of diabetic macular edema1) dostępna w Czytelni Medycznej Borgis. |
||||||||||||||||||||||||||||||||||||||||||||||
Chcesz być na bieżąco? Polub nas na Facebooku: strona Wydawnictwa na Facebooku |








