|
© Borgis - Postępy Nauk Medycznych 12, s. 901-903
*Ewa Czaplicka1, Iwona Grabska-Liberek2, Iwona Rospond1, Jarosław Kocięcki1
Zespół Tersona – omówienie przypadków klinicznych i postępowania leczniczego
Terson’s syndrome – case presentation and therapeutic management
1Department and Clinic of Ophthalmology, Poznań University of Medical Sciences
Head of Department and Clinic: Jarosław Kocięcki, MD, PhD 2Clinic of Ophthalmology, Medical Center of Postgraduate Education, Prof. W. Orłowski Independent Public Clinical Hospital, Warszawa Head of Clinic: Iwona Grabska-Liberek, MD, PhD, assoc. prof. Streszczenie
Zespół Tersona początkowo był definiowany jako krwotok do ciała szklistego powstały w związku z krwawieniem podpajęczynówkowym. Aktualnie na zespół ten składają się wszystkie przypadki krwotoków do wnętrza gałki ocznej, spowodowanych wewnątrzczaszkowym krwawieniem lub wzrostem ciśnienia wewnątrzczaszkowego. Krwotok wewnątrzgałkowy powstały w przebiegu zespołu Tersona może wystąpić jednostronnie lub w obojgu oczach. Może być zlokalizowany w przestrzeni podsiatkówkowej, śródsiatkówkowej, pomiędzy siatkówką a błoną graniczną ciała szklistego lub w komorze ciała szklistego. Diagnostyka różnicowa powinna obejmować wykluczenie innych przyczyn krwawienia wewnątrzgałkowego, takich jak: retinopatia cukrzycowa, zwyrodnienie plamki związane z wiekiem, guz wewnątrzgałkowy i odwarstwienie siatkówki o różnej etiologii. Autorzy prezentują trzy przypadki kliniczne zespołu Tersona, zdiagnozowane i leczone w Klinice Okulistyki Uniwersytetu Medycznego w Poznaniu. Dwa z nich miały przeprowadzoną witrektomię, jeden był leczony zachowawczo. Autorzy przedstawiają również wskazania i przeciwwskazania do leczenia chirurgicznego zespołu Tersona. Słowa kluczowe: zespół Tersona, witrektomia, sposoby leczenia krwotoku do ciała szklistego, krwotok wewnątrzczaszkowy, podwyższone ciśnienie śródczaszkowe
Summary
Terson’s syndrome initially was defined as intravitreal haemorrhage in combination with subarachnoideal bleeding. Presently the name of this syndrome comprises all cases of intraocular haemorrhages in the course of intracranial bleeding or intracranial hypertension. An intraocular haemorrhage appearing in the course of the Terson’s syndrome can be unilateral or bilateral. It may be localized in the subretinal space, intraretinaly, between the retina and limiting membrane of the vitreous or intravitreously. The differential diagnosis should encompass other causes of vitreous haemorrhage e.g. diabetic retinopathy, age-related macular degeneration, intraretinal tumor and retinal detachment of different etiology. The authors present 3 cases of Terson’s syndrome diagnosed and treated at the Department of Ophthalmology, University of Medical Sciences, Poznań, Poland. In 2 cases vitrectomy was performed, in 1 case a non-surgical therapy was administered. The authors present also indications and contraindications to the surgical management of Terson’s syndrome. Key words: Terson syndrome, treatment, vitrectomy, therapy modalities intravitreal haemorrhage, intracranial haemorrhage, intracranial hypertension
INTRODUCTION
The intraretinal haemorrhage in the course of a subarachnoid bleeding was first described in German literature by Litten in 1881 (1), but it is the description made by Terson in 1900 which is usually associated with this disease (2). Nowadays, the name also includes all forms of intraocular haemorrhage which can be associated with intracranial bleeding or intracranial hypertension (3, 4).
Clinical symptoms of Terson’s syndrome include a deterioration of visual acuity, which degree depends on the extent of the bleeding, along with characteristic neurological symptoms. Vitreous haemorrhage in the course of Terson’s syndrome can be unilateral or bilateral. Other clinical symptoms include optic disc oedema and formation of preretinal membranes in the macula region.
A differential diagnosis should encompass other causes of vitreous haemorrhage e.g. diabetic retinopathy, age-related macular degeneration, intraocular tumour or retinal detachment of different etiology.
Establishing a formal diagnosis and choosing a method of treatment requires computed tomography of the skull and/or magnetic resonance and, alternatively, a cerebrospinal fluid examination. A B-mode ultrasound scan allows for establishing the extent of haemorrhage and assessing the possibility of its spontaneous resorption. A close cooperation of ophthalmologist and neurologist is essential in the therapeutic process.
The aim of this work is to present 3 clinical cases of Terson’s syndrome, diagnosed and treated in the Clinic of Ophthalmology of the Poznan University of Medical Sciences.
DESCRIPTION OF CASES
Case No. 1 – G.B., female, 55 years old. Medical history: craniocerebral trauma, subdural haematoma of the frontoparietal region. Vitreous haemorrhage present in the exotropic left eye. The visual acuity before treatment was hand motion. Management: 6 months after the trauma – vitrectomy with SF6 gas application (VOS – 5/8 cc +3.0Dcyl ax 7) subsequently, a silicone oil endotamponade was applied due to retinal detachment (VOS in postoperative course up to 5/10 cc +8.0 sph) (fig. 1).
 Fig. 1. Image of left eye fundus after vitrectomy with silicone oil injection – case No. 1
Case No. 2 – K.M., male, 24 years old. Medical history: multiorgan trauma, subdural haematoma of the frontoparietal region on the right side. Vitreous bleeding in the right eye, preretinal membranes in the macular region and optic disc oedema. Visual acuity of the diseased eye was 5/50. Management: vitrectomy with silicone oil injection 5 months after the trauma, subsequently, the oil was removed after 6 months. Final visual acuity – 5/5.5 cc -1.0 Dcyl ax 50 (fig. 2).
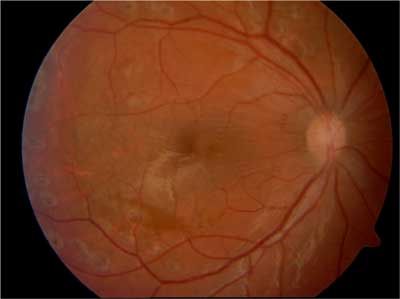 Fig. 2 Image of the right eye fundus after the removal of silicone oil – case No. 2.
Case No. 3 – C.T., male, 51 years old. Medical history: subarachnoid bleeding of unidentified etiology, haematoma located in posterior cranial fossa. Vitreous bleeding present in both eyes. The visual acuity before treatment was of hand motion level in both eyes. Management: observation – the general condition of the patient did not allow for local or general anaesthesia to perform surgery. In the course of approx. 14 months of observation, the visual acuity improved to 5/7 in the right eye and 5/5.5 in the left eye.
DISCUSSION
In the 3 clinical cases presented, the Terson’s syndrome occurred in the course of subdural bleeding resulting from craniocerebral trauma in 2 patients and in the course of subarachnoid bleeding of unidentified etiology in 1 patient. In 2 cases the vitreous haemorrhage was unilateral and in 1 case – bilateral. In 2 cases, due to no spontaneous resolution of the haemorrhage, a surgical treatment was performed while in 1 case the general condition of the patient made any surgical management impossible.
For many years, the mechanism of vitreous haemorrhage development in the course of Terson’s syndrome remained a matter of debate. One of the theories suggested that the bleeding spreads per continuum from the subarachnoid space, through the cribrum, to the vitreous chamber but electron microscopy and precise analysis of the optic nerve’s anatomy proved that there is no connection between these two spaces (3). Moreover, an analysis of histopathological preparations did not show any presence of blood elements between the optic nerve sheaths 3 mm from the eyeball. A second theory suggested that an abrupt increase of the intracranial pressure is transferred to the eyeball, causing an intraocular haemorrhage. This theory was disproved by experimental studies suggesting that in this instance, the venous pressure is not able to cause such a haemorrhage.
The most probable theory seems to be the one presuming that the primary cause of Terson’s syndrome is the elevation of intracranial pressure which causes oedema of the retrobulbar part of the optic nerve, which in turn hampers the venous return from retinal veins to cavernous sinus by closing the retinal and choroidal vessels on cribrum level. This creates a venostasis which causes minute superficial retinal vessels to rupture, resulting in vitreous bleeding. This theory also explains the occurrence of Terson’s syndrome in cases other than subarachnoid bleeding (3).
Currently, it is considered that the most common causes of Terson’s syndrome are aneurysms or vascular anomalies in the frontal part of the circle of Willis, usually concerning anterior communicating artery. Bleedings caused be these anomalies are considered to be responsible for the Terson’s syndrome in approx. 20-40% of cases (4, 5).
Currently available methods of treating the Terson’s syndrome include non-surgical therapy (placing the patient with a raised head, immobilizing the patient, withholding non-steroidal anti-inflammatory drugs, warfarin, anticoagulants and aspirin) and surgical management (argon laser photocoagulation in case of subretinal membranes and intraocular surgery). Spontaneous resorption of the haemorrhage can last for several months (according to some authors – 9 months on average) (3, 6, 7). No statistically significant difference has been found in the final visual acuity of patients treated with vitrectomy in comparison to patients in whom a spontaneous resorption of the haemorrhage occurred (7).
The indication for surgical management (pars plana vitrectomy) is a haemorrhage which was not absorbed for 3 months (3, 8) as well as:
– haemorrhage not undergoing resorption in monocular patients,
– haemorrhage in the premacular region,
– retinal detachment accompanying a haemorrhage,
– amblyopia prevention in children,
– late after-effects of intraocular haemorrhage (preretinal membranes, macular pucker),
– a vital need (e.g. due to the performed work) for a quick improvement of the visual acuity.
The contraindication are: low intensity haemorrhage with a high probability of spontaneous resorption and resorbing haemorrhage.
French authors who retrospectively assessed the efficacy of vitrectomy as a treatment method of the Terson’s syndrome remark that it is an efficient method in certain cases, however the distant prognosis of visual acuity is affected by numerous factors, not only distant complications characteristic for the Terson’s syndrome like formation of preretinal membranes (most common) but also complications of the vitrectomy itself (e.g. nuclear cataract or intraocular inflammation). They also describe an improvement of visual acuity after the treatment, with its stabilization in the 5th month. They also highlight that the final visual acuity is also affected by the neurological condition of the patient (e.g. accompanying damage to the brain structure, including the optic nerve atrophy). Additional factor which affects the prognosis negatively is age below 6 years (3, 6).
What lowers the availability of surgical treatment is, in some cases, the impossibility of general anaesthesia due to the grave condition of the patient. In such cases, the rarely-described argon laser treatment methods become an alternative e.g. facilitating the drainage of the contents of haematoma located premacularly in the subvitreal space to the vitreous chamber, by creating an opening in the posterior limiting membrane of the vitreous with subsequent destruction of the haemorrhage in the vitreous with Nd:YAG laser (9).
A method based on intravitreal administration of IgG anti-RhD class antibodies is an alternative for surgical treatment (3). Haemorrhage resorption in the vitreous depends on the haemolysis degree of erythrocytes. Administering IgG anti-RhD accelerates it and because the RhD antigens are specific for erythrocytes, the administration of antibodies does not cause damage to other tissues. However, this method can only be applied in Rh positive patients.
Summarizing, it is important to note that although the cause of Terson’s syndrome seems to be clearly identified, this disease can still pose a threat to patient’s sight and life and requires an individual approach to every patient. Piśmiennictwo
1. Litten M: Ueber einige vom allegmein-klinischen Standpunkt aus interessante Augenveranderungen. Berl Klin Wochnschr 1881; 18: 23-27.
2. Terson A: De l’hémorrhagie dans le corps vitre au cours de l’hémorrhagie cerebrale. Clin Ophthalmol 1900; 6: 309-312.
3. Nowosielska A, Czarnecki W: Zespół Tersona. Klinika Oczna 2003; 105(1-2): 79-81.
4. Nowosielska A, Czarnecki W, Ząbek M: Zespół Tersona w przebiegu tętniaków mózgu – obserwacje własne. Klinika Oczna 2003; 105(1-2): 49-51.
5. Biousse V, Newman NJ: Intracranial vascular abnormalities. Ophtalmology Clinics of North America 2001; 14: 243-264.
6. Quintyn JC, Massy J, Sanchez Ch, Brasseur G: Acuité visuelle finale des patients opérés par vitrectomie postérieure pour un syndrome de Terson. J Fr Ophtalmol 2000; 23(3): 221-224.
7. Schultz PN, Sobol WM, Weingeist TA: Long-term visual outcome in Terson syndrome. Ophthalmology Dec 1991; 98(12): 1814-1819.
8. Garweg JG, Koerner F: Outcome indicators for vitrectomy in Terson syndrome. Acta Ophthalmol Mar 2009; 87(2): 222-226.
9. Osoba Y, Talbot M: Indirect delivery of argon laser to disperse premacular haemorrhage in a recumbent visually handicapped patient with Terson’s syndrome. Eye 2000; 14(5): 800-802.
otrzymano/received: 2013-09-22 zaakceptowano/accepted: 2013-11-04 Adres/address: *Ewa Czaplicka Department and Clinic of Ophthalmology Autonomous Public Teaching Hospital no. 2, Poznan University of Medical Sciences ul. Długa 1/2, 68-848 Poznań tel.: +48 (61) 854-92-84 e-mail: dreczaplicka@gmail.com Artykuł Zespół Tersona – omówienie przypadków klinicznych i postępowania leczniczego w Czytelni Medycznej Borgis. |
Chcesz być na bieżąco? Polub nas na Facebooku: strona Wydawnictwa na Facebooku |








