|
© Borgis - Postępy Nauk Medycznych 12, s. 896-900
Irmina Jankowska-Lech1, *Iwona Grabska-Liberek1, Piotr Chojnowski1, Agnieszka Skowyra1, Jaromir Wasyluk2
Zmiany starcze aparatu ochronnego oka
Ageing of eye adnexa
1Clinic of Ophthalmology, Medical Center of Postgraduate Education, Warszawa
Head of Clinic: Iwona Grabska-Liberek, MD, PhD, assoc. prof. 2 Clinic of Ophthalmology, Military Institute of Aviation Medicine, Warszawa Head of Clinic: prof. Marek Prost, MD, PhD Streszczenie
Aparat ochronny oka stanowi niezwykle ważną część narządu wzroku, narażoną na ciągły wpływ świata zewnętrznego. Należą do niego: powieki wraz z łukami brwiowymi i rzęsami, spojówki powiek i gałki ocznej oraz narząd łzowy. W warunkach fizjologicznych zapewnia on stałą ochronę gałki ocznej przed szkodliwym działaniem czynników zewnętrznych, między innymi promieniowaniem ultrafioletowym czy różnego rodzaju urazami. Wraz z upływem czasu, aparat ochronny oka ulega procesowi starzenia, a więc zmniejsza się jego zdolność do samonaprawy będącej odpowiedzią na gromadzące się w wyniku stresu środowiskowego uszkodzenia wewnątrzkomórkowe. Może to prowadzić do utraty jego funkcji ochronnych, a w konsekwencji również nieprawidłowego funkcjonowania powierzchni oka. To z kolei może wpływać ostatecznie na obniżenie funkcji widzenia. Dlatego bardzo ważna jest wczesna diagnostyka tych zmian, monitorowanie ich przebiegu i w razie konieczności wdrożenie odpowiedniego leczenia, które miałoby na celu zapobieganie ich powikłaniom. Celem niniejszej pracy jest zestawienie i opisanie najważniejszych zmian starczych dotyczących poszczególnych elementów aparatu ochronnego oka. Słowa kluczowe: aparat ochronny oka, powieki, spojówka, narząd łzowy, zmiany starcze w narządzie wzroku
Summary
The eye adnexa is one of the most important parts of the organ of vision, which is permanently influenced by environmental factors. It consists of eyelids along with eyebrows and eyelashes, conjuctivas and eyeball and also lacrimal apparatus. In physiological conditions it constantly protect eyeball from harmful influence of external factors, i.a.: ultraviolet radiation or different kind of injuries. Over time the eye adnexa is effected by an aging process, therefore, its ability to selfrepair decrease on the grounds of intracellular damages caused by environmental stress factors. It may lose its protective functions and consequently cause an abnormal functioning of the ocular surface. At least it may decrease functions of vision. So, it is very important to diagnose this type of changes in early phase, control proceedings and implement apropriate treatment to prevent complications. The aim of this study is to compare and describe the major senile changes regarding the particular elements of the eye adnexa. Key words: eye adnexa, lids, conjuctiva, lacrimal organ, aging of visual organ
INTRODUCTION
Ageing is a natural, irreversible and intensifying process of changes in the metabolism and physicochemical properties of cells, which leads to an inhibition of autoregulation and regeneration of the body and to morphological and functional changes of its tissues and organs (according to the PWN Encyclopedia).
Eye adnexa is a group of tissues and anatomical structures which cover the eyeball and enable proper functioning of the eye. The eye adnexa consists of eyelids along with superciliary arches, palpebral and bulbar conjunctivae and lacrimal apparatus. The eyelids provide mechanical protection to the anterior part of the eyeball. Eyelashes and hair on the superciliary arch protect the eye from sweat and small particles. Apart from that, the eyelashes serve as sensors which trigger the eye-closing reflex. Blinking spreads tears across the anterior surface of the eye, moisturizing it. During blinking, a thin layer of tears is moved across the anterior surface of the cornea and the eyeball conjunctiva, washing any potential foreign bodies to the lower fold of lid conjunctiva and to the eyeball. Tear film creates a very smooth surface of the eyeball which allows the light to be properly refracted by the cornea, supplies the superficial layers of the cornea with oxygen as it does not have its own vessels. Tears have a slightly higher concentration of sodium chloride than other tissue fluids and, additionally. They contain small amounts of protein bodies with buffer capacity, as well as certain amount of lysozyme of antibacterial properties. Mechanical rinsing and the lysozyme protect the eye against infections.
SENILE CHANGES OF EYELIDS
The eyelid skin of elderly people is wrinkled. It is a result of dermis thinning, subcutaneous tissue atrophy, lowered elasticity and excessive skin dryness. The amount of lipids on the surface of skin is lowered parallel to the atrophy of lipids in the skin itself, which is caused by a significant drop in the number of fibroblasts synthesising and accumulating skin cholesterol. A lowered activity of sebaceous glands, especially in women, also takes place. In some people, a gland overgrowth occurs, which can lead to a formation of senile sebaceous adenomas.
A decrease in the skin’s elasticity and a lowered immunity of capillaries leads to their dilation (telangiectasia). A tendency to focal, brown discolourations (senile lentigines) occurs. In the case of both dry skin and seborrhoea, an increased tendency to inflammatory reactions occurs as a result of chemical, physical, thermal and bacterial factors.
The orbital fatty tissue atrophies in elderly people. The eyeball collapses and the palpebral fissure appears to be narrowed. A slow atrophy of the orbital septum can take place and the orbital fat can move forward (baggy eyelids). The eyeball sheath and palpebral ligaments become less elastic. The tarsus and eyelid muscles slowly atrophy which leads to a senile ptosis of the upper eyelid and to lower eyelid ectropion (fig. 1) (1). The treatment of the upper eyelid ptosis is based on a surgical correction under local anaesthesia and consists of cutting the palpebral sulcus, dissecting free the aponeurosis of the levator palpebrae superioris, suspending it to the tarsus and layer suturing.
 Fig. 1. Eyelid ectropion.
Eyelid ectropion causes the palpebral conjunctiva to become exposed. This leads to its hyperaemia, inflammatory overgrowth and epiphora. The latter is a consequence of lacrimation being increased by inflammation as well as by an impairment of the outflow of tears, which is a result of the lacrimal point (the first step of draining the tears) protruding out of the eyeball (2). The senile eyelid ectropion requires surgical correction which can be performed in 4 ways:
– tarsal-conjunctival resection: rhombus of approx. 3-4 mm vertically and 6-8 mm horizontally below the lacrimal point,
– “T” plastics: additional resection of a full-thickness pentagonal fragment of the eyelid, lateral from the lacrimal point,
– horizontal shortening of the eyelid: by resecting a proper, full-thickness fragment of the eyelid with an optional blepharoplasty of the lower eyelid,
– horizontal shortening of the eyelid: dissecting free, shortening and suspending the lateral palpebral ligament to the orbital margin periosteum (lateral tarsal strip) (fig. 2-7).
 Fig. 2. Lateral tarsal strip – before the surgical correction.
 Fig. 3. Lateral tarsal strip – the orbital rim periosteum.
 Fig. 4. Lateral tarsal strip – lateral ligament.
 Fig. 5. Lateral tarsal strip – 5.0 sutures to the orbital periosteum.
 Fig. 6. Lateral tarsal strip – reconstruction of lateral angle.
 Fig. 7. Lateral tarsal strip – 3 months after the surgical correction.
As a result of a constant or recurring contraction of the orbicular muscle of the eye a blepharospasm can occur (1).
Senile lower eyelid entropion is and effect of an excessive contraction of the sinews of ciliary part of the orbicular muscle (fig. 8). It rarely occurs before 40 years of age (1). As a consequence of lower eyelid entropion, an abnormal position of the ciliary margin towards the eyeball takes place and causes scraping of the corneal epithelium, creates defects in it and finally, as a result of an infection, deep ulcerations. The treatment for these types of palpebral changes is operative. Before the operation, the palpebral margin should be pulled away with an adhesive tape, stuck underneath the cilium and directed towards the cheek (2). There are two methods of surgical treatment of lower eyelid entropion, depending on the anatomic factors and the advancement of the entropion. The first method is cutting below the cilia line, resecting the excess of skin and orbicular muscle and layer suturing. The second method consists of lateral canthotomy and cantholysis, dissecting free the lower branch of the lateral ligament, suspending to the periosteum (the ligament or the tarsus – lateral tarsal strip), cutting out the excess of skin and eye orbicular muscle, reconstructing the external angle and layer suturing (to increase the lid’s horizontal tightness). Both operations are performed under local anaesthesia.
 Fig. 8. Eyelid entropion.
The aforementioned moving of the orbital towards the front or its falling out (steatoblepharon) results in an excess of eyelid skin (dermatochalasis). Although dermatochalasis is more frequent among elderly people, it can appear in middle-aged people, especially when family predisposition exists. Often in the course of dermatochalasis of the upper eyelid, an indistinct or lower-located palpebral fold occurs. Dermatochalasis can also accompany a true ptosis of upper eyelid. A significant excess of upper eyelid skin manifests itself as ailments of various types, such as heaviness around the eyes, eyebrow pains, obscuring of the vision axis by the eyelashes and ultimately leads to a limitation of the upper range of the field of vision. Often the vision deteriorates due to eyebrow ptosis, especially if the patient does not use the frontalis muscle to raise them and uncover the vision axis obstructed by the excess of skin. Lower eyelid dermatochalasis is regarded as a problem of cosmetic nature, until the excess of skin and moving of the orbital fat do not prevent the patient from having proper bifocal glasses selected (3). Then, the treatment is based on surgical correction – cutting out the excess of skin and subcutaneous tissue under local anaesthesia (fig. 9-12).
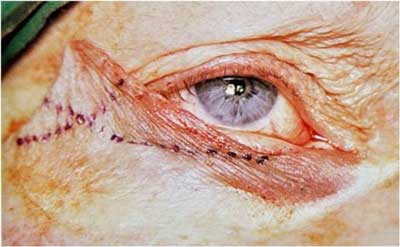 Fig. 9. Lower eyelid dermatochalasis – horizontal eyelid shortening.
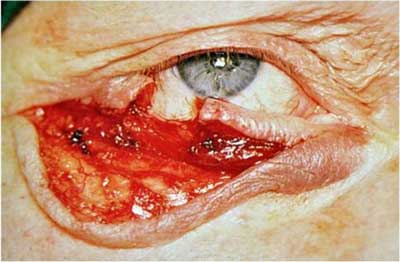 Fig. 10. Lower eyelid dermatochalasis – horizontal eyelid shortening.
 Fig. 11. Lower eyelid dermatochalasis – horizontal eyelid shortening.
 Fig. 12. Lower eyelid dermatochalasis – horizontal eyelid shortening.
In elderly people, palpebral neoplasms are observed more often, especially basal cell carcinoma (due to local malignancy referred to as epithelioma basocellulare). The basal cell carcinoma may occur in different forms. The nodular type is a hard, painless nodule, immovable in relation to deeper tissues (1) (fig. 13), the nodular ulcerative type is of heaped-up edge with central erosion; and the fibrosing type is an irregular plate without clearly visible borders which deforms the eyelid (2) (fig. 14). It is usually located next to the free margin of the lower eyelid, especially in the area of the medial angle. Remote metastases appear rarely, it can be locally malignant (1). The treatment of choice is an operational removal of the nodule with a 1-2 mm margin of healthy tissue.
 Fig. 13. Basal cell carcinoma – the nodular type.
 Fig. 14. Basal cell carcinoma – the fibrosing type.
In elderly people, metabolism-related palpebral diseases (depositary and degenerative) such as xanthelasma, also occur often (1).
Xanthelasma is a benign tumour on the eyelid skin in the form of flat, yellow bulges, usually in the area of the medial angle (fig. 15). Histologically, its cells are overfilled with cholesterol and other fatty bodies and it never displays a tendency for malignancy. It is treated due to cosmetic reasons and the treatment is either operative or with the use of CO2 laser or argon laser (2).
 Fig. 15. Xanthelasma.
SENILE CHANGES OF LACRIMAL APPARATUS
Over the years, the lacrimal gland becomes more visible. The amount of glandular tissue decreases while the amount of connective tissue increases. Many secretory vesicles atrophy, the number of plasma cells increases, pigment is accumulating in secretory cells and adipose degeneration takes place. The senile changes are also accompanied by a lowered secretion of tears. Their composition changes as well. The amount of cytokines increases, including inflammatory cytokines such as IL-6, 8, 12, TNF-α, EGF and MIP-1α. According to recent studies, the increased amount of inflammatory cytokines in the composition of tears causes eye irritation symptom, positive Schirmer’s test and defects in the epithelium of the cornea – typical dry eye symptoms (4).
Apart from the “artificial tears”, ciclosporin A and corticosteroids can be used generally. Patients aged 65-70 suffer from unspecified ailments such as photophobia and burning sensations in the eyes. These are accompanied by a secretion of sticky mucus and sometimes keratoconjunctivitis sicca can develop (1).
Often, due to senile eyelid ectropion, lacrimal point evorsion takes place, which leads to lacrimal point failure. Patients suffer from persistent lacrimation. Sometimes an accumulation of tears in the lacrimal lake is observed (1).
AGEING OF CONJUNCTIVA
The conjunctiva loses its transparency in different periods of life in each person. The epithelium thickens and desquamates in more exposed areas. The proper substance becomes thinner and less elastic. The conjunctival vessels can be more dilated in elderly people. Baggy telangiectasias, fusiform dilations and tortuous vessels appear. These changes do not occur in every person and are more expressed in the area of palpebral fissure. Moreover, an increased flaccidity in the area of inferior bulbar conjunctiva is often noticeable. This state, named conjunctivochalasis is characterised by an excessive, loose, non-oedematous conjunctiva between the lower eyelid and the eyeball (3).
CONCLUSIONS
Senile changes to the eye adnexa can lead to a loss of its physiological functions and consequently to ophthalmological disorders of different severity.
That is why an early diagnosis of these changes is crucial, as well as monitoring their course and applying proper treatment where necessary. Piśmiennictwo
1. Orłowski W: Okulistyka współczesna. Tom 2, Wydawnictwo lekarskie PZWL, Warszawa 1977: 643-687.
2. Niżankowska MH: Okulistyka. Podstawy kliniczne. Wydawnictwo lekarskie PZWL, Warszawa 2007: 128-137.
3. Basic and Clinical Science Course: Oczodół, powieki i układ łzowy (BCSC 7). I wyd. pol., Urban & Partner, Wrocław 2005: 239-371.
4. Lam H, Bleiden L, de Paiva CS et al.: Tear Cytokine Profiles in Dysfunctional Tear Syndrome. American Journal Of Ophthalmology 2009; 147: 198-205.
otrzymano/received: 2013-09-22 zaakceptowano/accepted: 2013-11-04 Adres/address: *Iwona Grabska-Liberek Clinic of Ophthalmology, Medical Center of Postgraduate Education Prof. W. Orłowski Independent Public Clinical Hospital ul. Czerniakowska 231, 00-416 Warszawa tel./fax: +48 (22) 629-71-09 e-mail: kl.okulistyki@szpital-orlowskiego.pl Artykuł Zmiany starcze aparatu ochronnego oka w Czytelni Medycznej Borgis. |
Chcesz być na bieżąco? Polub nas na Facebooku: strona Wydawnictwa na Facebooku |








