|
© Borgis - Postępy Nauk Medycznych 8, s. 617-622
*Grzegorz Madycki, Andrzej Gabrusiewicz, Paweł Dąbek, Walerian Staszkiewicz
Problemy w ultrasonograficznej ocenie miażdżycowych zwężeń tętnic szyjnych w Polsce
Problems in ultrasound diagnosis of atherosclerotic stenoses of the carotid arteries in Poland
Department of Vascular Surgery and Angiology of the Medical Centre for Postgraduate Education, The Jerzy Popiełuszko Memorial Bielański Hospital
Head of Department: prof. Walerian Staszkiewicz MD, PhD Streszczenie
Badanie ultrasonograficzne tętnic szyjnych jest obecnie uważane za podstawowe w diagnostyce patologii tętnic szyjnych. W większości rekomendacji oraz prowadzonych badań uwzględniających chorobę miażdżycową tętnic szyjnych jest ono uznawane za podstawowe i zazwyczaj jedyne tak w diagnostyce, jak i w leczeniu. Głównym celem badania ultrasonograficznego tętnic szyjnych i kręgowych jest rozpoznanie, bądź wykluczenie patologii w obrębie tych naczyń. Autorzy w poniższej pracy przedstawiają główne problemy związane z odpowiednią interpretacją wyniku, prawidłową techniką samego badania, oraz różne aspekty związane implikacjami wynikającymi z rozpoznania zmian w tętnicach szyjnych (wskazania do operacji, odpowiednie kwalifikowanie, itp.). W podsumowaniu, Autorzy zwrócili uwagę, iż wykonujący badanie ultrasonograficzne i opisujący wynik tego badania, muszą mieć świadomość, iż może ono skutkować decyzją o leczeniu zachowawczym, bądź o operacyjnym chorego. Każda z tych strategii nie jest wolna od ograniczeń i w przypadku wyniku USG rozbieżnego od stanu faktycznego, skutkować może błędną strategią leczenia, o potencjalnie groźnych dla chorego skutkach. Słowa kluczowe: miażdżyca, tętnice szyjne, USG
Summary
The ultrasound evaluation of the carotid arteries is currently considered as the basic examination in diagnostics of pathology of the carotid arteries. In most recommendations and conducted studies on atherosclerosis of the carotid arteries, it is recognized as the main tool in diagnostics and in planning the treatment strategy. The main purpose of the ultrasound evaluation of the carotid and vertebral arteries is confirming or ruling out the pathology within these vessels. Authors of this paper present the main problems related to interpretation of vascular exam, the correct examination technique and various implications directly linked to the obtained diagnosis of the carotid pathology (indications for an invasive treatment, adequate qualification process). In conclusion, they make a point that the ultrasound exam of the carotid arteries may result in the decision to treat each individual patient with conservative or surgical method. None of the strategies implicated is free from limitations and complications. Therefore, a false ultrasound diagnosis may result in wrong decision making regarding treatment strategy, which may be potentially fatal to the patient. Key words: atherosclerosis, carotid arteries, ultrasound
Introduction
Currently in Poland, ultrasound evaluation of the carotid arteries is performed practically by physicians of all specialties, without possibility to evaluate their experience in this particular area.
We observe that not only persons certified by Polish Ultrasound Society (not recognized in the European Union legislation), but also persons with specialties, which require skills in performing ultrasound evaluation of the vessels: radiology, angiology and vascular surgery, claim the right to perform these exams.
The problem of accurate interpretation of the result of the carotid artery ultrasound evaluation may be suitably perceived by mentioned groups of physicians, but performing these evaluations by physicians, who do not have any qualifications, but just benefiting from confusion and increasing demand for performing these evaluations, is becoming much more serious problem.
An additional problem is the fact that majority of persons is not involved in broadly defined vascular pathology and are not able to follow the progress, which took place during the last decade in reference to knowledge on pathophysiology of the diseases of the carotid arteries. We also have to remember that this examination decides on treatment method, which may prevent the cerebrovascular accident/death of the patient, or put the patient at unnecessary risk of these events.
Therefore, diversity of the groups performing these examinations leads to an assumption that instead of limiting and checking competencies, more important would be creation of some competencies in terms of ultrasound evaluation of the carotid arteries and accept certain standards, which should be binding.
For this reason, it seems to be necessary to bring up the problems of standardization of the ultrasound evaluation of the carotid arteries – which is the subject discussed for almost 20 years, and despite this fact, it is still open: i.a. in reference to advances in knowledge on the carotid arteries pathophysiology.
The ultrasound evaluation of the carotid arteries is currently recognized as the basic one in diagnostics of the carotid arteries pathology. In majority of recommendations and conducted studies considering the atherosclerosis of the carotid arteries, it is recognized as the basic one and usually the only one not only in diagnostics, but also in treatment. In the U.S., as early as in 2001, Medicare announced that in over 80% of the patients undergoing surgical treatment of the carotid arteries stenosis, the only qualifying evaluation was ultrasound examination (1).
The main purpose of the ultrasound evaluation of the carotid and vertebral arteries is confirming or ruling out the pathology within these vessels. For this reason, by ordering ultrasound evaluation we expect that the examination will allow us classifying the patients to one of the following subgroups (these more significant):
– Patients without significant pathological lesions.
– Patients with insignificant intensity of lesions (< 50% decrease in diameter of the vessel), who should be conservatively treated if any symptoms occur.
– Patients with more advanced lesions (stenosis between 50% and 70% in diameter of the vessel), whose first-line treatment should be conservative, while monitoring progress of the disease, especially occurrence of the neurological symptoms.
– Patients with significantly advanced lesions (> 70% decrease in the lumen of the vessel), in reference to whom the surgical treatment should be first considered.
– Patients with total closure of the lumen of the vessel, who are currently qualified for conservative therapy, as the first-line treatment (this qualification may be changed in specific rare cases).
There is no data in Poland, which evaluate frequency of qualification for surgery of the carotid arteries based on ultrasound evaluation alone – however, it should be assumed that it significantly exceeds 90%. It creates significant implications in terms of standardization of the examination and controversies related to some of its elements.
Significant aspects of the ultrasound evaluation of the carotid arteries:
1. Method of evaluation of the degree of stenosis.
2. Technique of the evaluation itself (kinking).
3. Technique of the evaluation of the Doppler spectrum.
4. Interpretation and use of selected parameters of the flow velocity spectra and their indices.
5. Morphological image of the atherosclerotic lesions.
Method of evaluation of the degree of stenosis
Key element of the examination includes evaluation of the stenosis degree. ACAS study (asymptomatic patients) demonstrated that within the group of patients without neurological deficit, number of patients needed to be treated, i.e. to prevent the cerebrovascular accident in patients with 50% stenosis, was 68. It means that performing 136 procedures of restoring patency of the carotid arteries in these patients, will allow preventing as little as 2 the cerebrovascular accidents within the period of 2 years, at the most (2, 3). Similar results were achieved in comparable Veterans Affairs trial. No study until NASCET and ECST trials allowed preparing certain, preliminary standards of evaluation of the degree of stenosis (4-6).
Unfortunately, indications prepared for both trials simultaneously became source of basic misunderstanding, causing incomparability of the simultaneously conducted ultrasound evaluations. As figure 1 presents, one method was used to calculate the degree of stenosis in NASCET trial, and another one was used in ECST trial (7).
 Fig. 1. Method of measuring the degree of stenosis in NASCET trial, and in ECST trial.
Degree of stenosis according to measurement in NASCET trial corresponded to the following degree of stenosis obtained in measurement in ECST trial (tab. 1).
Table 1. Comparison of the degree of stenosis obtained in NASCET and ECST trials, respectively.
Figure 2 presents linear relationship between measurements of the degree of stenosis: Currently recommended criterion for evaluation of the degree of stenosis is NASCET criterion, which is also accepted in the United Kingdom (7).
 Fig. 2. Discrepancies between obtained degree of stenosis resulted from various methods of measurement in NASCET and ECST trials (see fig. 1 and tab. 1).
It should be remembered that measurements were initially conducted based on angiographic evaluations, and then ultrasound evaluation was implemented (studies lasted over many years), which obviously resulted in different criteria for evaluation of stenoses based on velocity.
Significant factor, which is not currently considered in discussions over precision of ultrasound measurements conducted at the turn of the 80’s and the 90’s was poor resolution of ultrasound machines and usually no ability to use technique of color encoding for the flow (so-called “color Doppler”). These limitations, which did not provide opportunity to visualize hypoechogenic lesions (these the most susceptible to destabilization and neurological symptoms) enforced use, as the only criterion: changes in flow velocity.
Difference in quality of lesion imaging – at the left there is an image of the lesion in the carotid artery provided by the ultrasound machine of 2000-2005, at the right, there is an image from the machine of older generation (the 90’s) (fig. 3, 4).
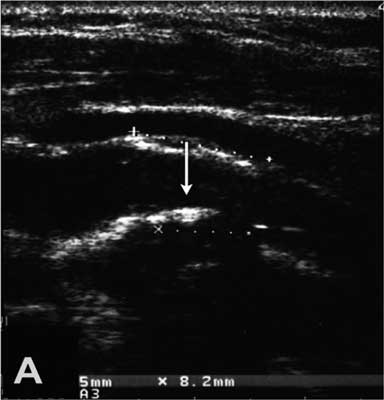 Fig. 3. Image the bifurcation of the carotid artery provided by the machine used in the 90’s.
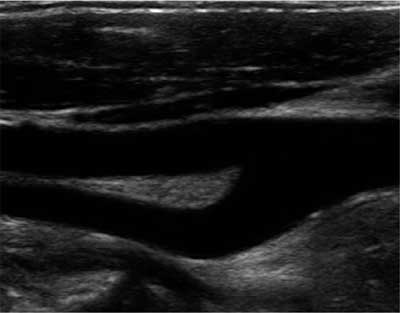 Fig. 4. Image the bifurcation of the carotid artery provided by the machine of the newest generation.
Results of NASCET and ECST trials are “distorted” in natural way by not considering hypoechogenic lesions – invisible in ultrasound machines of old generations.
Technique of evaluation
Required heads: linear with frequency of at least 7.5 MHz and convex (5 MHz); the second one for evaluating the distal segment of the internal carotid artery. Except for evaluation of the common carotid arteries, the bulbs, and origins of the internal and external carotid arteries and vertebral arteries, the following should always be done:
– evaluation of the distal segment of the brachiocephalic trunk with the site of bifurcation into the subclavian artery and the right common carotid artery,
– imaging the intracranial segment of the internal carotid artery. This part of evaluation is extremely important (in this case, the convex head is very useful), because it facilitates determination of highly located atherosclerotic lesions in the internal carotid artery or looping,
– evaluation of the bulb: it was demonstrated that large atherosclerotic lesions in large bulbs (measuring > 10 mm in diameter) – despite maintained wide lumen of the flow, constitute a significant risk factor for microembolization (8). This factor has not been considered at all in NASCET trial (similarly to the problem of unstable atherosclerotic lesions),
– evaluation of the width of the vessels (especially important in females). It should be considered whether the arteries are not narrow. Width of the internal carotid arteries below 5 mm or looping is a significant clue for the surgeon in terms of the type of the procedure that should have to be done (placing a patch in case of a narrow artery or reimplantation in case of looping) (fig. 5, 6).
 Fig. 5. Image of the double angulation [kinking] of the internal carotid artery.
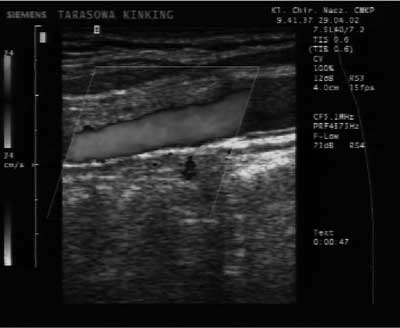 Fig. 6. Image of normal origin of the internal carotid artery – in CD option.
Evaluation of significance of the atherosclerotic lesions
The atherosclerotic lesions may be described as:
– mild (in case of stenosis < 50% according to NASCET; excluding massive lesions in large bulbs of the common carotid arteries and hypoechogenic lesions – recognized as high risk lesions),
– advanced (stenosis > 50% according to NASCET, hemodynamically significant lesions, massive lesions in large bulbs, hypoechogenic lesions, or potential ulcerations of the lesion surfaces).
Doppler spectrum of the carotid arteries is different: each examining physician should have knowledge about this fact. Flow in the internal carotid artery is typically low-resistant flow (low values of PI, high RI) as opposed to the flow in the external carotid artery (highly resistant flow with high values of PI, and low RI); in the artery, which is proximally patent, but highly occluded in a distal segment (e.g. under the base of the skull, the blood inflows and outflows: it causes extremely highly resistant flow with short increasing waves and amplitude lowering, the positive values (inflow) are equal to the negative values (outflow) (fig. 7, 8).
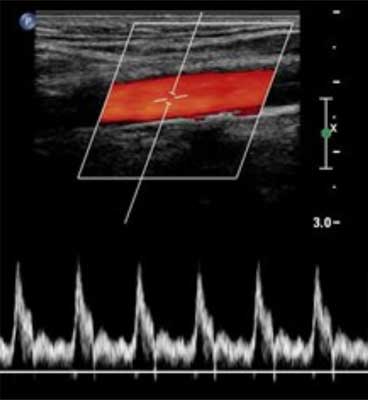 Fig. 7. Low-resistant flow – typical for the internal carotid artery.
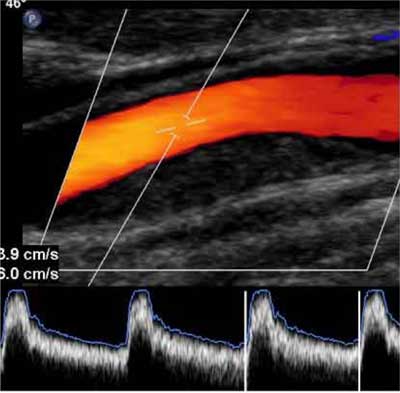 Fig. 8. Moderately low-resistant flow – typical for the common carotid artery.
Velocity values: they still remain the basic criterion for evaluation of the degree of stenosis. Here is high variety of criteria evaluating this degree based on: peak systolic velocity (PSV), end-diastolic velocity (EDV) as well as PSV and EDV indices. Only in NASCET trial, 6 criteria were developed for evaluation of the degree of stenosis based on lesions in velocity values (9) – see the table 2.
For this reason, it is important to unify criteria in a given study center or provide information, according to what criteria the degree of stenosis was evaluated.
Doppler beam crossing angle
Values of the peak systolic velocity as well as end-diastolic velocity significantly change depending on the beam crossing angle – the lower the angle, the lower flow values (10, 11). Optimal value for the angle is 45-60° (fig. 9). The attention has also to be paid to correct placement of the Doppler gate with selection of the angle suitable to the direction of the flow lumen (12).
 Fig. 9. The diagram showing correct placement of the Doppler gate: (A) in the eccentric lesion (parallel to the stream flow) and (B) the gate placed correctly to the lumen, which is not pathologically changed (8).
Morphological image of the atherosclerotic lesions
In order to inform the reader, an important seems to be reminding the basic concepts related to the most frequently diagnosed disease, i.e. atherosclerosis. The atherosclerosis begins in early childhood, but it takes a few decades of life for development and evolution of the atherosclerotic plaques responsible for neurological symptoms. While we observe the plaque development related to proliferation of the smooth muscles, the matrix synthesis and lipid accumulation, which is the whole process leading to stenosis of the vessel, we have to take into consideration that in majority of the patients with atherosclerotic stenosis of the carotid arteries, in principle, this process is asymptomatic. It may be undoubtedly stated that atherosclerotic process is a mild disease in this (majority) group of patients. This is significantly important, because it relates to the cerebral circulation, which is circulation with significant compensative abilities. To a large extent, the fact that severe lesions are not hemodynamically significant (it relates to the low resistance of the cerebral circulation and compensation from the other side, which is efficient in over 86% of the patients), definitely differentiates atherosclerotic lesions in the carotid arteries from lesions in other locations. In majority (> 85%) of the patients, microembolization caused by releasing embolic material from the unstable atherosclerotic lesions, or their total disintegration, resulted in thrombus in the artery, is the reason for occurrence of neurological complications.
Problem of stability/instability of the atherosclerotic lesions in the carotid arteries has been studied for about 20 years. It was defined for the first time in 1991 (13), and attempts of morphological evaluation of the atherosclerotic lesions in the carotid arteries using ultrasound examination was comprehended over 12 years ago.
Summary
Physicians performing the ultrasound evaluation and describing its result have to be aware that this result may lead to a decision on conservative or surgical treatment of a patient. None of these strategies is free from limitations and if ultrasound evaluation result is inconsistent with actual condition, it may result in inaccurate treatment strategy with results, which are potentially dangerous for the patient (14). Therefore, description of each evaluation should include as much information included in the table 2 as possible.
Table. 2. Information, which should be included in report of the carotid arteries evaluation.
Piśmiennictwo
1. Grant EG, Benson CB, Moneta GL et al.: Carotid artery stenosis: gray-scale and Doppler US diagnosis – Society of Radiologists in Ultrasound Consensus Conference. Radiology 2003; 229: 340-346.
2. Barnett HJ, Eliasziw M, Meldrum HE, Taylor DW: Do the facts and figures warrant a 10-fold increase in the performance of carotid endarterectomy on asymptomatic patients? Neurology 1996; 46: 603-608.
3. Mayo SW, Eldrup-Jorgensen J, Lucas FL et al.: Carotid endarterectomy after NASCET and ACAS: a statewide study. North American Symptomatic Carotid Endarterectomy Trial. Asymptomatic Carotid Artery Stenosis Study. J Vasc Surg 1998; 27: 1017-1022.
4. Barnett HJ, Taylor DW, Eliasziw M et al.: Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 1998; 339(20): 1415-1425.
5. Rothwell PM, Gutnikov SA, Warlow CP: European Carotid Surgery Trialist’s Collaboration. Reanalysis of the final results of the European Carotid Surgery Trial. Stroke 2003; 34(2): 514-523.
6. North American Symptomatic Carotid Endarterectomy Trial Collabolators. Beneficial Effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 1991; 325: 445-453.
7. Rothwell PM, Pendlebury ST, Wardlaw J, Warlow CP: Critical appraisal of the design and reporting of studies of imaging and measurement of carotid stenosis. Stroke 2000; 31(6): 1444-1450.
8. Oates CP, Naylor A, Hartshorne T et al.: Joint Recommendations for Reporting Carotid Ultrasound Investigations in the United Kingdom – review. Eur J Vasc Endovasc Surg 2009; 37: 251-261.
9. Eliasziw M, Rankin RN, Fox AJ et al.: Accuracy and prognostic consequences of ultrasonography in identifying severe carotid artery stenosis. North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. Stroke 1995; 26(10): 1747-1752.
10. Tola M, Yurdakul M: Effect of Doppler angle in diagnosis of internal carotid artery stenosis. J Ultrasound Med 2006; 25: 1187-1192.
11. Nowak J, Jogestrand T: Duplex ultrasonography is an efficient diagnostic tool for the detection of moderate to severe internal carotid artery stenosis. Clin Physiol Funct Imaging 2007; 27: 144-147.
12. Cole S: (ed.) Vascular Laboratory Practice: Part 2 Extra- and intracranial arterial assessment. Institute of Physics and Engineering in Medicine. York 2001.
13. Ross R: Atherosclerosis – an inflammatory disease. N Engl J Med 1999; 340(2): 115-125.
14. Braun RM, Bertino RE, Milbrandt J et al.: Ultrasound imaging of carotid artery stenosis: application of the Society of Radiologists in Ultrasound Consensus Criteria to a Single Institution Clinical Practice. Ultrasound Q 2008; 24: 161-166.
otrzymano/received: 2012-05-14 zaakceptowano/accepted: 2012-06-11 Adres/address: *Grzegorz Madycki Department of Vascular Surgery and Angiology Medical Centre for Postgraduate Education The Jerzy Popiełuszko Memorial Bielański Hospital ul. Cegłowska 80, 01-809 Warszawa tel.: +48 (22) 569-02-85 e-mail: g.madycki@interia.pl Artykuł Problemy w ultrasonograficznej ocenie miażdżycowych zwężeń tętnic szyjnych w Polsce w Czytelni Medycznej Borgis. |
Chcesz być na bieżąco? Polub nas na Facebooku: strona Wydawnictwa na Facebooku |








