|
© Borgis - Postępy Nauk Medycznych 8, s. 531-535
*Agnieszka Brodzisz1, Czesław Cielecki2, Paweł Nachulewicz2, Paweł Wieczorek1
Zastosowanie ultrasonografii przezkroczowej i endosonografii z zastosowaniem H2O2 w diagnostyce ropni i przetok okołoodbytniczych u dzieci
The use of transperineal ultrasound and endosonography using H2O2 in the diagnosis of perianal abscesses and fistulas in children
1Department of Pediatric Radiology, Medical University, Lublin
Head of Department: prof. Paweł Wieczorek, MD, PhD 2Department of Surgery and Pediatric Traumatology, Medical University, Lublin Head of Department: Paweł Nachulewicz, MD, PhD Streszczenie
Wstęp. Ropnie okołoodbytnicze u dzieci nie są zmianami rzadkimi, a patogeneza przetoki nie jest do końca wyjaśniona. Najczęściej leczenie chirurgiczne polega na nacięciu ropnia i ewakuacji jego treści oraz rewizji jamy ropnia bez stosowania metod obrazowych. Ultrasonografia przezkroczowa, jak i badanie endosonograficzne wysokiej częstotliwości w trybie obrazowania 3D pozwalają na ocenę rozległości i penetracji ropni oraz przetok okołoodbytniczych. Cel. Celem pracy jest ocena przydatności ultrasonografii przezkroczowej oraz endosonografii z zastosowaniem wody utlenionej w ocenie rozległości ropni i przetok okołoodbytniczych u dzieci. Materiał i metody. Badanie USG wykonano u 9 dzieci w wieku od 2 miesiąca do 8 lat z ropniem i przetoką okołoodbytniczą. Badanie wykonywano przed nacięciem ropnia, oceniając jego rozległość oraz po jego nacięciu po podaniu wody utlenionej w celu oceny kanału przetoki. Badanie wykonywano aparatami USG: Philips iU22 głowicami wysokiej częstotliwości L 12-5 Mhz i L 15-7 Mhz oraz BK profocus głowicą rotacyjną 20-52 o częstotliwości 16-9 Mhz z 360-stopniową akwizycją danych pracującą w trybie 3D. Wyniki. U wszystkich badanych pacjentów ropnie i przetoki okołoodbytnicze w badaniu USG w skali szarości były statystycznie istotnie mniejsze aniżeli po badaniu z użyciem H2O2. Badanie kontrastowe u wszystkich badanych pozwoliło na uwidocznienie dystrybucji i relacji anatomicznych do zwieraczy wewnętrznego i zewnętrznego odbytu i poszerzenie rozległości zabiegu operacyjnego. U wszystkich pacjentów uzyskano ustąpienie ropnia, zagojenie przetoki oraz brak nawrotu w krótkotrwałej obserwacji. Wnioski. Badanie USG z dojścia przezkroczowego i przezodbytniczego pozwoliło na ocenę rozległości ropni i przetok okołoodbytniczych i rozszerzenie zabiegu. Słowa kluczowe: ultrasonografia przezkroczowa, endosonografia, ropień i przetoka okołoodbytnicza u dzieci
Summary
Introduction. Perianal abscesses are not uncommon pathology in children, while the ethiopathology of perianal fistula still need to be determined. Surgical treatment involves abscess incision and evacuation usually without the need for imaging. Transperineal ultrasound (TPUS) and endorectal ultrasound (ERUS) enable the assessment of the distribution and penetration of perianal abscesses and fistulas. Aim. Aim of this study is the evaluation of usefulness of the intrasurgical TPUS and H2O2 enhanced endosonography in the assessment of the distribution and penetration of perianal abscesses and fistulas in children. Material and methods. US examination was performed in 9 children (aged 2 month to 8 years old) with perianal abscess and fistula. The examination was performed before abscess incision in order to assess its distribution, as well as after surgical incision, and H2O2 injection to visualise fistulous tract. The US examinations were performed with the use of Philips iU22 ultrasound scanner with high frequency transducers (L 12-5 MHz and L 15-7 MHz) and BK-Medical Profocus ultrasound scanner with high frequency (16-9 MHz) 360 degrees rotational transducer with automatic 3D data acquisition (type 2050). Results. The measurements of perianal abscesses and fistulas in all patients taken at B-mode US were statistically significantly lower than that ones taken after H2O2 injection. H2O2 enhanced US examination enabled precise assessment of anatomical relations between abscesses and fistulous tracts towards external and internal anal sphincters influencing widening of the extent of surgery. Surgical treatment was successful in all patients. No recurrence was noticed in short time follow-up. Conclusions. Transperineal and transanal US with the use of high frequency transducers and H2O2 injection enabled precise assessment of the distribution of perianal abscesses and fistulas, and had an impact on the surgery extent. Key words: transperineal ultrasound, endorectal ultrasound, perianal abscesses and fistula in children
Introduction
The exact incidence of perianal abscesses (perinealabscess, PA) and fistulas (fistula-in-ano, FIA) in the pediatric population is not known. Large statistical reports, including both adults and children indicate that children constitute between 0.5 and 4% of all patients (1). More than 80% of all patients with PA/and the FIA are children under one year of age, boys: girls – 9:1 (1). The etiology of perianal abscesses/fistulas is not entirely clear. There are several theories explaining the development of the PA/FIA: anal gland inflammation, anoderm infection, anal fissure infection, congenital abnormal cells of the intestinal wall anchor in the anoderm (2). The presence of perianal abscesses and fistulas in childhood almost exclusively concern boys to 1 year of age, and therefore emphasizes the influence of prenatal androgens on the development of abnormal glands of Morgagni of the anal canal designed to deepen and cause thinning of the anal crypts (3). Compared to adults, there are significant differences in anatomy, etiology, statistics or treatments for PA/FIA. During infancy pelvis is shallower in the longitudinal dimension, and the length of the anal canal is approximately 5 mm. Fistula is a straight line according to Goodsall’s rule, almost all of them are of a low intersphincteric type, according to Parks’ classification in adults, this type constitutes 70% (4), external parts of fistulas are usually located at “9” and “3”and lying in litothomy position. In children, the disease was only local, with no signs of systemic infection. Factors predisposing to the development of PA/FIA are: lowered immunity, diabetes, hematologic malignancies, granulomatous disease (5, 6).
All these factors determine the diversity of not only therapeutic but also diagnostic conduct in children at this age. In diagnostic imaging of perianal abscesses and fistulas great role is played by ultrasound (7). With access through the perineum – transperineal ultrasound (TPUS) and endoscopic (endorectal) examination (ERUS). The use of conventional endorectal probes in infants is limitedby the above-mentioned anatomical conditions, and therefore transperineal ultrasound examinations are carried out (8). TPUS examinations can be performed with conventional probes with frequency 2-6 MH, linear probe with frequency 5-10 MHz or end-fire probes used for endosonography. ERUS examination is performed in older children (sometimes in sedation) using a radial electronic probe or a mechanical rotationalhead. TPUS and ERUS examinations allow to evaluate the anatomy of the anal canal and perianal area area, as well as anatomy of sphincters, and in the presence of a fistula, their relationship (9). Spatial imaging (3D) in ERUS and TPUS examinations allows better assessment of the extent and penetration of perianal abscesses and fistulas (10). But not always performing a gray-scale ultrasound allows the assessment of the extent of the abscess and the course of the canal or multiple canals of fistula. Therefore the administration of hydrogen peroxide (H2O2) is helpful in confirming the diagnosis, in determining the course of the canal or multiple canals of fistula and in the assessment of the internal opening of fistulas (11).
Aim
The purpose of this paper is to evaluate the usefulness of ultrasonography and transperineal endosonography using hydrogen peroxide (H2O2) in assessing the extent of perineal abscesses and fistulas in children.
Material and methods
The study group consisted of nine children with abscess and/or perianal fistula diagnosed and treated in the Department of Pediatric Surgery and Department of Children Radiology of the Medical University in Lublin. The age of children ranged from 2 to 8 years (the mean 4 years), including 5 children in infancy, all boys. In all children an ultrasound examination of soft tissues around the abscess and transperineal examinations were performed. In addition, endoscopic ultrasound of the anal canal was performed in four children aged 3 to 8 years. Surgery was performed under general intravenous anesthesia, using perioperative intravenous antibiotics. In the litothomy patient positioning after the identification and location of the lesion (PA/FIA) in ultrasound examination incision and evacuation of the contents of the abscess were performed. Then, under ultrasound guidance, and the administration of hydrogen peroxide (H2O2) the presence and extent of the fistula canal or canals were assessed. In the presence of abscess and fistula, fistulotomy on the probe ring canal set under ultrasound guidance was performed simultaneously with the evacuation of the abscess.
Ultrasonography was performed with ultrasound systems: Philips and U22, high frequency probes L 12-5 MHz and L 15-7 MHz, convex 5-8 MHz and BK Pro-Focus rotationalhead 2050 with frequency 16-9 MHz with 360 degrees data acquisition in 3D mode.
Results
In the analyzed group of nine children, the ultrasound abscess and fistula (PA/FIA) were observed in 6 of them (67%), in 3 patients (33%) only the abscess was observed. In all patients perianal abscess was located under the skin at the anal verge, in five children on the right side, in four on the left side. In patients with the presence of perianal abscess and fistula in 5 of them opening of the fistula was located at 9, in 1 patient at 3 hours. In the ultrasound examination, all patients had the typical hipoechogenic appearance of the abscess area, in 6 subjects with an irregular outline. In the largest cross-sectional size the abscesses ranged from 8 x 7 mm to 25 x 30 mm. In three subjects soft tissue swelling was present around the abscess showing no blood flow signal. In 3 (50%) children transperinalgray-scale ultrasound showed a single fistula canal clearly visible in a form of a hypoechoic, narrow linear structure, in one (17%) there were hypoechoic, tubular structures with tortuosity corresponding to shallow subcutaneous fistulas. In two (33%) infants transperinal gray-scale ultrasound did not show fistula canal. In a group of 4 subjects who underwent additional 3D ERUS in 1 patient fistula penetration in the direction of the prostate was found (fig. 1, 1a). The administration of hydrogen peroxide (H2O2) to the external mouth of fistula confirmed its presence in all 6 patients (fig. 2, 2a), including 2 (33%) with complex fistula. Ultrasound examination with the administration of hydrogen peroxide also allowed the identification in all six children the internal opening of fistula around the crypt. In 5 (83%) children fistulas had a shallow subcutaneous course, in 1 (17%) boy an intersphincteric one.
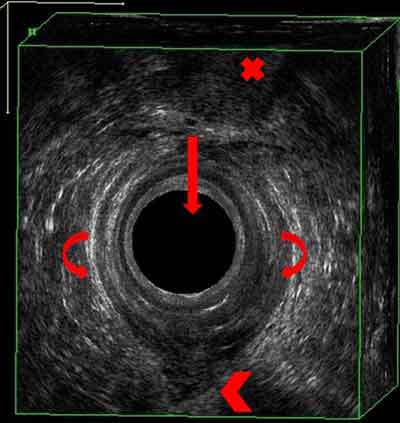 Fig. 1. Transrectal ultrasound, rotary head type 2050 16-9 MHz. Arrow-head in the anal canal, the tip-hypoechoic abscess, curved arrows-internal anal sphincter, the tag-prostate gland.
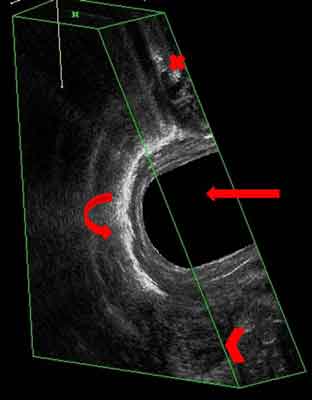 Fig. 1a. Transrectal ultrasound, rotary head type 2050, 16-9 MHz after the administration of H2O2. Arrow-head in the anal canal, the tip-hypoechoic abscess, curved arrows-the presence of H2O2 in the fistula canal penetrating into the prostate-gland, the tag prostate gland.
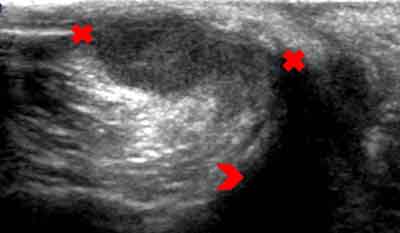 Fig. 2. Transperineal ultrasound, linear head L 12-5 MHz, cross-section. Tags-hypoechoic abscess; tip-anal canal.
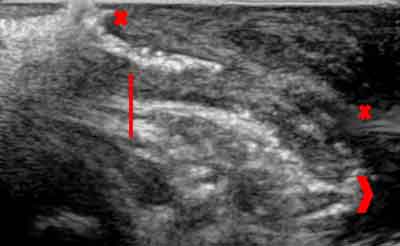 Fig. 2a. Transperineal ultrasound, linear head L 12-5 MHz longitudinal section after the administration of H2O2. Tags-abscess, arrow – hyperechoic reflection-the presence of H2O2 in the fistula channel, tip-anal canal.
Discussion
Perianal abscesses (perinealabscess, PA) and fistulas (fistula-in-ano, FIA) in children are rare and the exact incidence is not well known (1). The differences mainly related to anatomy and etiology between adults and children do not in a simple manner allow to transfer the methods of diagnosis and treatment from adults onto the pediatric population (10). In children, most of the procedures are performed under general anesthesia and the following are applied: aspiration, incision and drainage of abscess, fistulotomia, rarely fistulectomia. Recent reports also indicate the possibility of conservative management or minimally invasive one involving the aspiration of the abscess (12), what is a result of the lack of generalized inflammation in children as well as proven possibility of spontaneous healing or closing the fistula canal as the child grows.
In surgical procedure for PA/FIA the most important element is to identify the internal opening of fistula in the corresponding crypt and the very course of fistula canal (17). “Blind” probing the abscess cavity and the external mouth of fistula in the search for a canal may lead to a false path due to the fragility of infiltration tissue and the natural laxity of children (13). Performing fistulotomy along the false path can lead to the recurrence of the fistula and additional branching with the risk of the inflammatory process spreading into deep perineal structures (11). Therefore, the evaluation of perianal abscesses and fistulas in children before operation and during intraoperative procedures with TPUS and ERUS ultrasound studies seems right. In the adult population with inflammatory perianal changes those examinations have been carried out for a long time and have a high diagnostic efficacy (7,15), however they are not routinely performed in the pediatric population. Transperinal ultrasound in children is performed mainly in the diagnosis of congenital anal anomalies and accompanying fistulas (14,16) and transrectal examination is performed only in difficult diagnostic cases in older children. TPUS and ERUS examinations with 3D acquisition provide important information on the structure of the anal canal, the location of the abscess and the presence of fistulas and their relationship with respect to the anal sphincters. The use of H2O2 also allows better visualization of the fistula canal and any of its branching, and what is very important, the assessment of the internal opening. 3D ultrasound of the anal canal performed in older children allows for obtaining a block of tissue covering the entire anal canal with the ability to assess individual layers in three different planes.
In the analyzed group of nine children performed TPUS and ERUS ultrasound allowed for an accurate assessment of the size and location of the abscess. In 4 patients they allowed a better identification of the fistula canal, including 2 patients with fistula branching, and the location of the internal opening. In one boy 3D endoscopic ultrasound enabled the diagnosis of fistula penetrating into the prostate gland. The administration of hydrogen peroxide (H2O2) by the external mouth of fistulas significantly improved their identification, the assessment of their course and the internal opening. In two children with transperineal gray-scale ultrasound showing no fistula, the administration of hydrogen peroxide allowed its identification.
The analyzed material includes a small number of children and you cannot determine the sensitivity and specificity of the research, nevertheless in the opinion of the authors described techniques are an important contribution to a better assessment of perianal abscesses and fistulas in children, and therefore the treatment.
Conclusions
1. Pre- and intraoperative transrectal and transperineal ultrasound allowed a better assessment of the extent of perineal abscesses and fistulas and the choice of surgical technique.
2. Additional administration of a contrast being hydrogen peroxide into the external mouth of the fistula allows for precise visualization of the course and the anatomical relationship to the internal and external anal sphincters.
3. In all patients the resolution of the abscess, fistula healing and no recurrence were achieved. Piśmiennictwo
1. Festen C, Hat-ten van H: Perianal Abscess and fistula-in-ano in infants. J Pediatr Surg 1998; 33: 711-713.
2. Afsarlar CE, Karaman A, Tan?r G et al.: Perianal abscess and fistula-in-ano in children: clinical characteristic, management and outcome. Pediatr Surg Int 2011; 27: 1063-1068.
3. Murthi GVS, Okoye BO, Spicer RD et al.: Perianal abscess in childhood. Pediatr Surg Int 2002; 18: 689-691.
4. Billingham R, Isler J: The diagnosis and management of common anorectal disorders. Curr Probl Surg 2004; 41: 586-645.
5. Piazza DJ, Radhakrishnan J: Perianal abscess and fistula-in-ano in children. Dis Colon Rectum 1990; 33: 1014-1016.
6. Serour F, Gorenstein A: A characteristics of perianal abscess and fistula-in-ano in healthy children. World J Surg 2006; 30: 467-472.
7. Sudoł-Szopińska I, Kołodziejczak M, Jakubowski W: Ultrasonografia przezodbytnicza w diagnostyce chorób proktologicznych. Medycyna Rodzinna 2005; 1: 4-8.
8. Littlewood-Tell R, Share JC: Transperinealsonography in children. American Journal of Roentgenology 1997; 168: 1263-1267.
9. Wieczorek AP, Woźniak MM, Stankiewicz A: Ultrasonografphy. [In:] Wieczorek AP, Bartram CI, Santoro GA (eds.): Pelvic floor disorders: imaging and multidisciplinary approach to management. Dordrecht, Springers 2010: 175-187.
10. Sudoł-Szopińska I, Kołodziejczak M, Jakubowski W, Stefański R: Przydatność przezodbytniczej ultrasonografii trójwymiarowej w diagnostyce chorób proktologicznych. Medycyna Rodzinna 2003; 2: 89-93.
11. Ziech M, Felt-Bersmar R, Stoker J: Imaging of Perianal Fistulas. Clinical Gastroenterology and Hepatology 2009; 7: 1037-1045.
12. Serour F, Somekh E, Gorenstein A: Perianal abscess and fistula-in-ano in infants: a different entity? Dis Colon Rectum 2005; 48: 359-364.
13. Macdonald A, Wilson-Storey D, Munro F: Treatment of perianal abscess and fistula-in-ano in children. Br J Surg 2003; 90: 220-221.
14. Haber HP, Seitz G, Warmann SW, Fuchs J: Transperineal sonography for determination of the type of imperforate anus. AJR 2007; 189: 1525-1529.
15. Sudoł-Szopińska I, Szczepkowski M, Kołodziejczak M et al.: Przydatność endosonografii ze wzmocnieniem kontrastowym w diagnostyce przetok odbytu. Medycyna Rodzinna 2004; 3: 113-116.
16. Choi YH, Kim In-One MD, Cheon J-E et al.: Imperforate Anus: Determination of Type Using Transperineal Ultrasonography. Korean J Radiol 2009; 10: 355-360.
17. King S, Beasley S (eds.): Should we seek a fistula-in-ano when draining a perianal abscess? J Ped Child Health 2010; 46: 273-274.
otrzymano/received: 2013-05-15 zaakceptowano/accepted: 2013-06-26 Adres/address: *Agnieszka Brodzisz Department of Pediatric Radiology Medical University ul. Chodźki 2, 20-093 Lublin tel.: +48 817-418-447 e-mail: abrodzisz@wp.pl Artykuł Zastosowanie ultrasonografii przezkroczowej i endosonografii z zastosowaniem H2O2 w diagnostyce ropni i przetok okołoodbytniczych u dzieci w Czytelni Medycznej Borgis. |
Chcesz być na bieżąco? Polub nas na Facebooku: strona Wydawnictwa na Facebooku |








